Sources: The Complete Pug by James Trullinger; petmd.com; Pug Dog Club of America; American Kennel Club; our personal vets over the years and 3 and 1/2 decades of pug owning experience
Table of Contents - on this webpage:
PET POISON NUMBER: (855) 764-7661
Pet Poison Helpline, (If you think your pug ate your medicine or something weird that you know it ate this will help the er vets as they don't know the answer to all things and pet poison can help decide if you need to go to ER and then even help the ER formulate a plan.)
Online Chocolate Toxicity Calculator (to help you decide if your pet ate enough chocolate to warrant an emergency): https://www.vetcalculators.com/chocolate.html
1st Aid Kit
Handling the Dog for Treatment - Administering Pills and Liquid Meds
Bites and Wounds
Allergies
Walking Dandruff
Hot Spots
Demodectic Mange
Yeast Infections
Staff Infections
Burns
Swallowing Foreign Objects or Poisoning
Shock
Constipation
Diarrhea
Pneumonia (including aspiration pneumonia)
Dog Acne
Ear Infections
Eye Injuries
Entropion
Corneal Ulcers
Dystichia
Proptosis
Brachycephalic Airway Syndrome
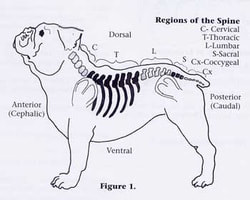
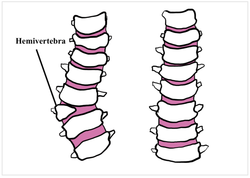
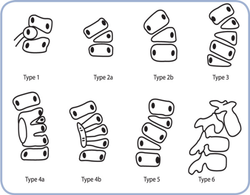
Pug Orthapedics
Hemivertebrae
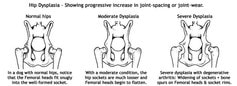
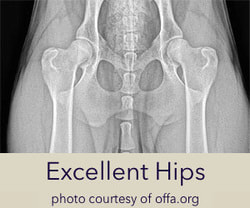
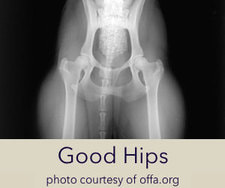
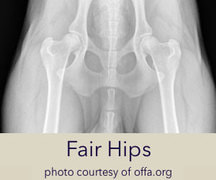
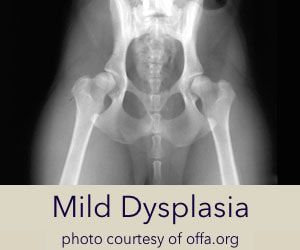
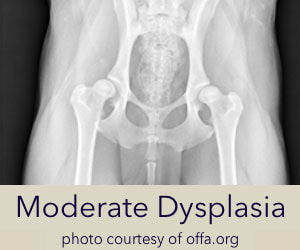
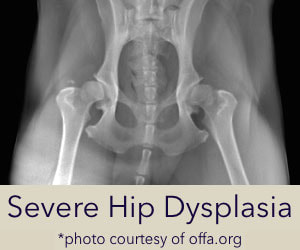
Hip Dysplasia
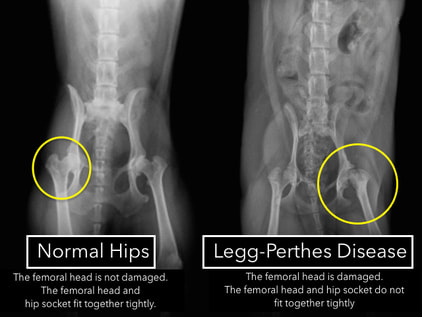
Legg-Perthes
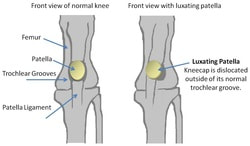
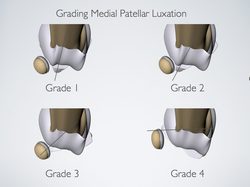
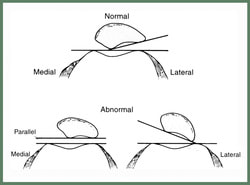
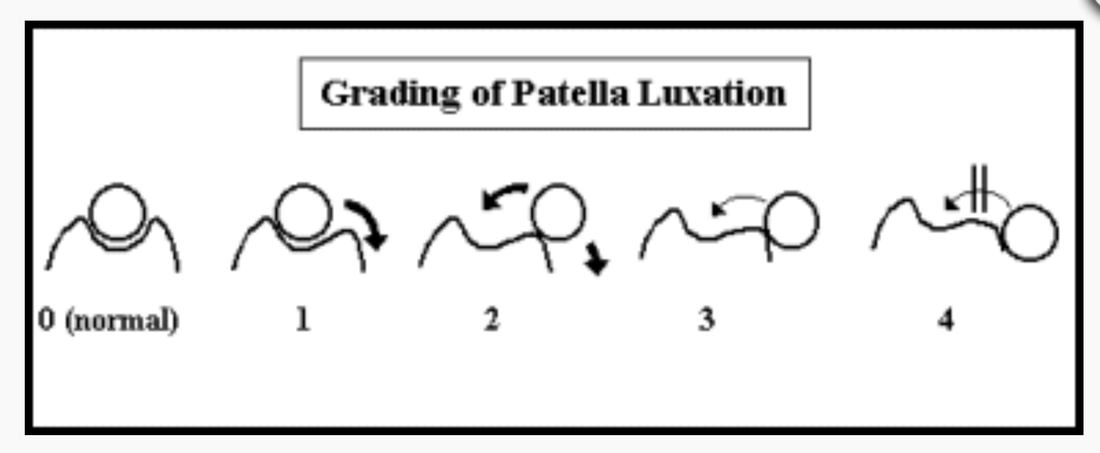
Luxating Patellas
Pug Myelopathy
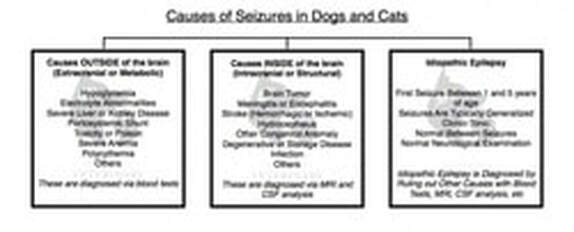
Epilepsy
Pug Dog Encephalitis
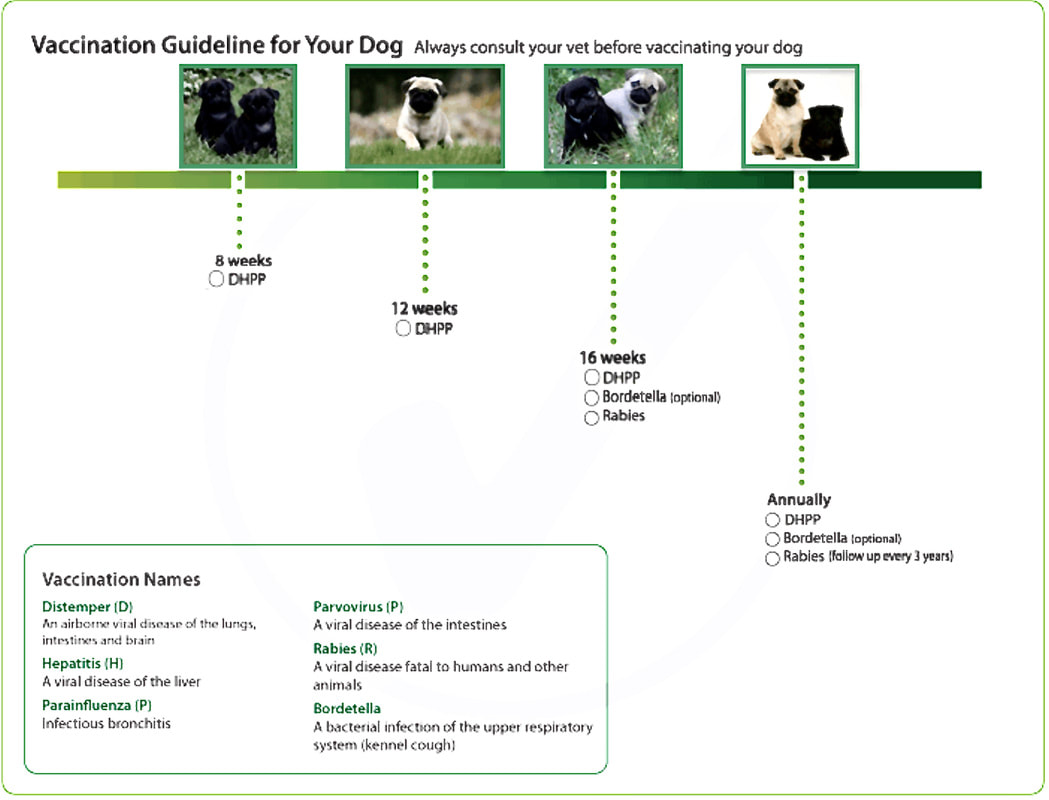
Vaccinations
Porcupines and Skunks
PET POISON NUMBER: (855) 764-7661
Pet Poison Helpline, (If you think your pug ate your medicine or something weird that you know it ate this will help the er vets as they don't know the answer to all things and pet poison can help decide if you need to go to ER and then even help the ER formulate a plan.)
Online Chocolate Toxicity Calculator (to help you decide if your pet ate enough chocolate to warrant an emergency): https://www.vetcalculators.com/chocolate.html
1st Aid Kit
Handling the Dog for Treatment - Administering Pills and Liquid Meds
Bites and Wounds
Allergies
Walking Dandruff
Hot Spots
Demodectic Mange
Yeast Infections
Staff Infections
Burns
Swallowing Foreign Objects or Poisoning
Shock
Constipation
Diarrhea
Pneumonia (including aspiration pneumonia)
Dog Acne
Ear Infections
Eye Injuries
Entropion
Corneal Ulcers
Dystichia
Proptosis
Brachycephalic Airway Syndrome
Pug Orthapedics
Hemivertebrae
Hip Dysplasia
Legg-Perthes
Luxating Patellas
Pug Myelopathy
Epilepsy
Pug Dog Encephalitis
Vaccinations
Porcupines and Skunks
"As in human medicine, most treatment and dosing of dogs are better left in the experienced, trained hands and mind of a professional (veterinarian). However, there are times and situations when professional aid is not immediately available and an owner's prompt action may save a life or avoid permanent injury. To this purpose, the following suggestions are given." -- The Complete Pug, James Trullinger
Here is a great resource if your vet is unavailable (because most problems occur late at night or on a Sunday, right? ha)
Online Symptom Checker (Caution: As our vet tech is always saying, beware of Dr. Google -- don't necessarily jump to the worst case scenarios -- but sometimes it is difficult to know when you should rush to the vet, and when you should wait a bit.)
Here is a great resource if your vet is unavailable (because most problems occur late at night or on a Sunday, right? ha)
Online Symptom Checker (Caution: As our vet tech is always saying, beware of Dr. Google -- don't necessarily jump to the worst case scenarios -- but sometimes it is difficult to know when you should rush to the vet, and when you should wait a bit.)
The 1st Aid Kit
Teramycin ointment for eyes
pair of tweezers
pair of pliers
straight scissors
rectal thermometer
magnifying glass
syringes
flashlight
towel
teaspoon
tablespoon
cotton swab
Dressings: cotton balls, roll of cotton, roll of 2" gauze
nonstick bandages
adhesive tape
Strips of clean, old sheets may come in handy
antiseptic spray
ammonia
listerine
benadryl (we have tablets -- typically use about 1/2 a tablet)
(aspirin - our vet has advised us not to use this)
brandy
3% hydrogen peroxide
baking soda (bicarbonate of soda)
Pepto-Bismal (milk of bismuth) or Milk of Magnesia
kaopectate
mineral oil
salt
tea
vaseline
baby oil
baby powder
baby wipes
scissors
Forticep Blue Butter (surgical scrub)
Wound dressing gel
Chlorhexidine wipes
or
Chlorhexidine liquid solution (as per Veterinarian Dr. Rachael Scariano, and owner of a Pickwick pug, "a great antiseptic option. You can use as a foot soak if they have redness or a wound on the paw, or anywhere except the eyes. You dilute it a bit with warm water ... it doesn't burn like alcohol and is more soothing. People always seem to use hydrogen peroxide for wounds and it actually delays wound healing ... I have seen awful wounds just worsened from hydrogen peroxide.")
Eye wash (or saline solution)
We like to have tramadol and some other rx medicines from our vet on hand. Talk to your vet about adding some of these rx to your 1st aid kit.
Some other things that are nice to have:
stethoscope
nebulizer
syringe bulb
cool mist humidifier
heating pad
Soft Elizabethan Collar
soft muzzle
extra leash/collar
collapsible travel water bowl
emergency packets for heat (or cold)
Teramycin ointment for eyes
pair of tweezers
pair of pliers
straight scissors
rectal thermometer
magnifying glass
syringes
flashlight
towel
teaspoon
tablespoon
cotton swab
Dressings: cotton balls, roll of cotton, roll of 2" gauze
nonstick bandages
adhesive tape
Strips of clean, old sheets may come in handy
antiseptic spray
ammonia
listerine
benadryl (we have tablets -- typically use about 1/2 a tablet)
(aspirin - our vet has advised us not to use this)
brandy
3% hydrogen peroxide
baking soda (bicarbonate of soda)
Pepto-Bismal (milk of bismuth) or Milk of Magnesia
kaopectate
mineral oil
salt
tea
vaseline
baby oil
baby powder
baby wipes
scissors
Forticep Blue Butter (surgical scrub)
Wound dressing gel
Chlorhexidine wipes
or
Chlorhexidine liquid solution (as per Veterinarian Dr. Rachael Scariano, and owner of a Pickwick pug, "a great antiseptic option. You can use as a foot soak if they have redness or a wound on the paw, or anywhere except the eyes. You dilute it a bit with warm water ... it doesn't burn like alcohol and is more soothing. People always seem to use hydrogen peroxide for wounds and it actually delays wound healing ... I have seen awful wounds just worsened from hydrogen peroxide.")
Eye wash (or saline solution)
We like to have tramadol and some other rx medicines from our vet on hand. Talk to your vet about adding some of these rx to your 1st aid kit.
Some other things that are nice to have:
stethoscope
nebulizer
syringe bulb
cool mist humidifier
heating pad
Soft Elizabethan Collar
soft muzzle
extra leash/collar
collapsible travel water bowl
emergency packets for heat (or cold)
Handling the Dog for Treatment
"Approach any injured or sick dog calmly with reassuring voice and gentle, steady hands. If the dog is in pain, slip a gauze or sheet strip noose over its muzzle" (we have a muzzle for pugs) "tying the ends first under the throat and then back of the neck. Make sure the dog's lips are not caught between his teeth, but make noose around muzzle tight."
If the dog needs to be moved, grasp the loose skin on the back of the neck with one hand and support chest with the other hand. If the dog is too large to move in this manner, slide him on a large towel, blanket or folded sheet which may serve as a stretcher for two to carry."
"If a pill or liquid is to be administered, back the dog in a corner in a sitting position. For a pill, pry back of jaws apart with thumb and forefinger of one hand and with the same fingers of your other hand place pill as far back in dog's throat as possible; close and hold jaws, rubbing throat to cause swallowing (holding head up). If dog does not gulp, hold one hand over nostrils briefly; he will gulp for air and swallow pill. If swallowing liquids, lift the back of the upper lip and tip spoon (or insert syringe into cheek area) into the natural pocket formed in the rear of the lower lip; it may be necessary to pull this pocket out with forefinger. Do not give liquids by pouring directly down the dog's throat; this might choke him or make the fluid go down the wrong way" (so that the pug aspirates into lungs).
"After treatment keep dog quiet, preferably in his bed or a room where he cannot injure himself or objects."
"Approach any injured or sick dog calmly with reassuring voice and gentle, steady hands. If the dog is in pain, slip a gauze or sheet strip noose over its muzzle" (we have a muzzle for pugs) "tying the ends first under the throat and then back of the neck. Make sure the dog's lips are not caught between his teeth, but make noose around muzzle tight."
If the dog needs to be moved, grasp the loose skin on the back of the neck with one hand and support chest with the other hand. If the dog is too large to move in this manner, slide him on a large towel, blanket or folded sheet which may serve as a stretcher for two to carry."
"If a pill or liquid is to be administered, back the dog in a corner in a sitting position. For a pill, pry back of jaws apart with thumb and forefinger of one hand and with the same fingers of your other hand place pill as far back in dog's throat as possible; close and hold jaws, rubbing throat to cause swallowing (holding head up). If dog does not gulp, hold one hand over nostrils briefly; he will gulp for air and swallow pill. If swallowing liquids, lift the back of the upper lip and tip spoon (or insert syringe into cheek area) into the natural pocket formed in the rear of the lower lip; it may be necessary to pull this pocket out with forefinger. Do not give liquids by pouring directly down the dog's throat; this might choke him or make the fluid go down the wrong way" (so that the pug aspirates into lungs).
"After treatment keep dog quiet, preferably in his bed or a room where he cannot injure himself or objects."
Bites and Wounds
If dog is in pain, or has a mild allergic reaction to, say, sting by an insect, and if you see any swelling anywhere, give Benadryl®, also known by its generic name, diphenhydramine, is one of the few over-the-counter drugs designed for people that veterinarians may have pet parents administer at home. But while Benadryl® is generally well tolerated by dogs and has a wide safety margin, it’s not necessarily the answer to your dog’s issue. If the pug seems in pain you can administer the correct dose of tramadol or rx your vet has prescribed for your 1st aid kit.
According to the Merck Veterinary Manual, the standard dose for Benadryl® is 2–4 milligrams per kilogram of body weight, or 0.9–1.8 milligrams (mg) of Benadryl® per pound. Therefore, a simple and practical dose is 1 mg of Benadryl® per pound of your dog's weight, given two to three times a day.
If dog is in pain, or has a mild allergic reaction to, say, sting by an insect, and if you see any swelling anywhere, give Benadryl®, also known by its generic name, diphenhydramine, is one of the few over-the-counter drugs designed for people that veterinarians may have pet parents administer at home. But while Benadryl® is generally well tolerated by dogs and has a wide safety margin, it’s not necessarily the answer to your dog’s issue. If the pug seems in pain you can administer the correct dose of tramadol or rx your vet has prescribed for your 1st aid kit.
According to the Merck Veterinary Manual, the standard dose for Benadryl® is 2–4 milligrams per kilogram of body weight, or 0.9–1.8 milligrams (mg) of Benadryl® per pound. Therefore, a simple and practical dose is 1 mg of Benadryl® per pound of your dog's weight, given two to three times a day.
This was our KK after she had an allergic reaction to something outside (we don't know what) -- perhaps an insect sting. It happened FAST (and of course Jeff was home alone, Amy was out of town). Luckily, it was the middle of a weekday and we live a block away from our vet so they worked us in. However, most emergencies seem to happen late at night on a Sunday, right? If you are in the middle of the woods camping and this happened, that's when that benadryl in the 1st aid kit would come in handy until you could get to the vet. (Yes, don't forget to pack that 1st aid kit when traveling!)
So, if your pug is in pain, or has a mild allergic reaction (hopefully, not as bad as KK's!) to, say, a sting by an insect, and if you see any swelling anywhere, give Benadryl®, also known by its generic name, diphenhydramine, is one of the few over-the-counter drugs designed for people that veterinarians may have pet parents administer at home. But while Benadryl® is generally well tolerated by dogs and has a wide safety margin, it’s not necessarily the answer to your dog’s issue. If the pug seems in pain you can administer the correct dose of tramadol or rx your vet has prescribed for your 1st aid kit.
If it's an obvious bite or wound, you can clip hair from area if it's hard to see. (With some double pug coats it's more challenging than others). Professional Heavy Duty Dog Grooming Clipper 3-Speed - https://amzn.to/2G6Mv0i
Wash gently with pure soap and water. If profuse bleeding continues, apply sheet strip or gauze tourniquet between wound and heart but nearest the wound. Release the tourniquet briefly at 10 minute intervals. Cold water compresses may stop milder bleeding. Once bleeding is under control, apply antiseptic spray or the blue gel and wrap again.
Chlorhexidine liquid solution (as per Veterinarian Dr. Rachael Scariano, and owner of a Pickwick pug, "a great antiseptic option. You can use as a foot soak if they have redness or a wound on the paw, or anywhere except the eyes. You dilute it a bit with warm water ... it doesn't burn like alcohol and is more soothing. People always seem to use hydrogen peroxide for wounds and it actually delays wound healing ... I have seen awful wounds just worsened from hydrogen peroxide.")
For insect bites and stings, try to remove stinger with tweezers or a dab of cotton then apply antiseptic -- The Complete Pug by James Trullenger
If it's an obvious bite or wound, you can clip hair from area if it's hard to see. (With some double pug coats it's more challenging than others). Professional Heavy Duty Dog Grooming Clipper 3-Speed - https://amzn.to/2G6Mv0i
Wash gently with pure soap and water. If profuse bleeding continues, apply sheet strip or gauze tourniquet between wound and heart but nearest the wound. Release the tourniquet briefly at 10 minute intervals. Cold water compresses may stop milder bleeding. Once bleeding is under control, apply antiseptic spray or the blue gel and wrap again.
Chlorhexidine liquid solution (as per Veterinarian Dr. Rachael Scariano, and owner of a Pickwick pug, "a great antiseptic option. You can use as a foot soak if they have redness or a wound on the paw, or anywhere except the eyes. You dilute it a bit with warm water ... it doesn't burn like alcohol and is more soothing. People always seem to use hydrogen peroxide for wounds and it actually delays wound healing ... I have seen awful wounds just worsened from hydrogen peroxide.")
For insect bites and stings, try to remove stinger with tweezers or a dab of cotton then apply antiseptic -- The Complete Pug by James Trullenger
When our All-American, Lexi, (a golden retriever, chow, dachshund mix) was bitten by a snake, we rushed to the first vet who could take us. We were lucky. Here is a guide to snake bites in dogs.
Swallowing Foreign Objects
If object is still in mouth or throat, reach in and remove it. If swallowed, give strong salt solution as for poisoning. Some objects that are small, smooth or soft may not give trouble. There can be problems with making a pug vomit, however, (aspiration pneumonia), so contact your vet first if possible. Amy's mother's Japanese Chin died quickly after swallowing a potasium pill that was dropped accidentally. So, sometimes, expediency is important.
Poisoning
If container of the poison is handy, use recommended antidote printed theron. Otherwise, make a strong solution of household salt in water (or hydrogen peroxide) and force into the dog's throat using the lip pocket method. Minutes count with severa poisons; if veterinarian cannot be reached immediately, try to get dog to an emergency vet or MD or registered nurse.
If object is still in mouth or throat, reach in and remove it. If swallowed, give strong salt solution as for poisoning. Some objects that are small, smooth or soft may not give trouble. There can be problems with making a pug vomit, however, (aspiration pneumonia), so contact your vet first if possible. Amy's mother's Japanese Chin died quickly after swallowing a potasium pill that was dropped accidentally. So, sometimes, expediency is important.
Poisoning
If container of the poison is handy, use recommended antidote printed theron. Otherwise, make a strong solution of household salt in water (or hydrogen peroxide) and force into the dog's throat using the lip pocket method. Minutes count with severa poisons; if veterinarian cannot be reached immediately, try to get dog to an emergency vet or MD or registered nurse.
Shock
If your pug has chewed an electric cord, protect your hand with rubber glove or thick dry towel and pull cord from socket. If your pug has collapsed, hold amonia under its nose or apply artificial respiration as follows: place the pug on side with its head low, press on abdomen and rib cage, releasing pressure at one or two second intervals. KEEP PUG WARM.
If your pug has chewed an electric cord, protect your hand with rubber glove or thick dry towel and pull cord from socket. If your pug has collapsed, hold amonia under its nose or apply artificial respiration as follows: place the pug on side with its head low, press on abdomen and rib cage, releasing pressure at one or two second intervals. KEEP PUG WARM.
Allergies
Some Pugs can get seasonal allergies. They often are quite itchy and sometimes chew their feet. This can start out during a limited time of the year but it can also expand to problems year round. Sometimes antihistamines, steroids and special shampoos are needed. A veterinary dermatologist can test your dog to see what the offending substances are and make up special allergy injections to desensitize your dog. Food allergies aren’t terribly common but a trial on a hypoallergenic diet might be ordered by your vet. Over decades of owning/fostering/breeding 100s of pugs we have dealt with 2 pugs with food allergies (eggs) and others with seasonal allergies. Cytapoint shots help tremendously.
Some Pugs can get seasonal allergies. They often are quite itchy and sometimes chew their feet. This can start out during a limited time of the year but it can also expand to problems year round. Sometimes antihistamines, steroids and special shampoos are needed. A veterinary dermatologist can test your dog to see what the offending substances are and make up special allergy injections to desensitize your dog. Food allergies aren’t terribly common but a trial on a hypoallergenic diet might be ordered by your vet. Over decades of owning/fostering/breeding 100s of pugs we have dealt with 2 pugs with food allergies (eggs) and others with seasonal allergies. Cytapoint shots help tremendously.
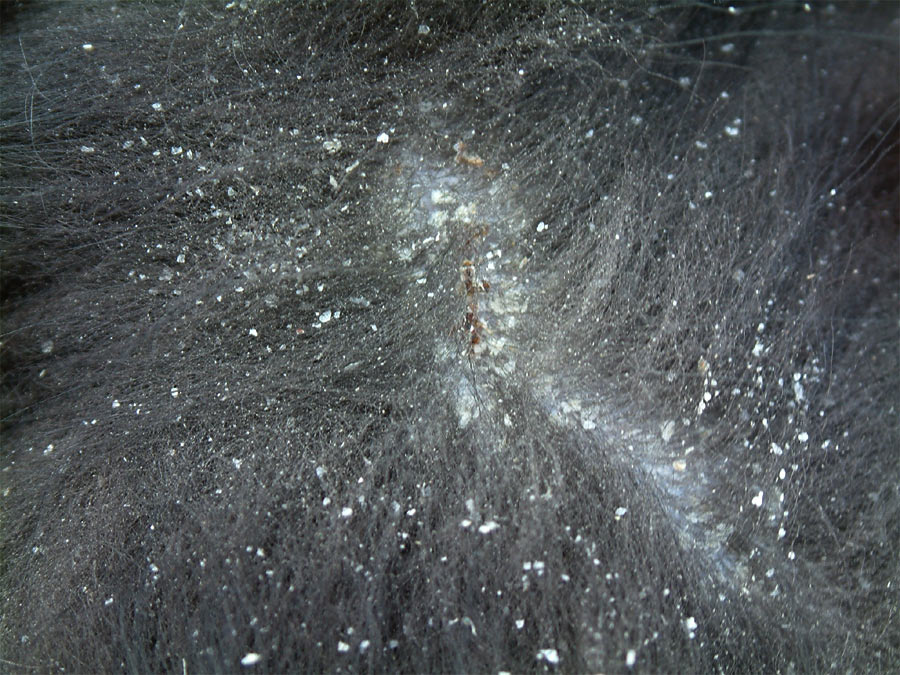
Walking Dandruff (Cheyletiellosis) is a skin condition which seems to be gaining interest among Pug people. It is caused by a small mite and results in very heavy scaling, dandruff and scurf, especially down the middle of the back. It can be itchy and can also cause crusts to form. The mite is notoriously hard to find. If you suspect your Pug has dandruff in excess of what might be seen with dry skin, your vet can comb off some of the flakes onto a microscope slide with a drop of mineral oil on it and look for the mites or the eggs under the microscope. Alternatively, the vet can press sticky tape against the skin and put the tape on a slide to view. Cheyletiella is very contagious so if mites are found or the disease is considered likely, all the pets must be treated for four weeks. You and your vet can discuss the options, some of which include flea shampoo or spray or ivermectin given orally or subcutaneously. Another good choice is topical Revolution every 15 days for 3 treatments. You also must treat the environment and clean any grooming equipment, too. There can be asymptomatic carriers so it is important to treat all pets. The most dramatic cases I have seen involved young puppies, with very thick closely adhered white flakes all along their backs. The prognosis is good but of course there is potential for re-infestation. See your vet if you think any of your Pugs might have these mites.
Hot Spots
Out of all the possible skin conditions in dogs, hot spots are among the most common. Hot spots can have different underlying causes and treatments based on severity.
Hot spots, also known as acute moist dermatitis, are painful red areas of infected skin that appear to be irritated and are sometimes raised.
Hot spots on dogs can occur anywhere on the body, but they are commonly found on the face, neck, limbs, or hips. The size and appearance of the lesions can vary slightly in each location, but most will look similar regardless of where they are. These spots can appear quickly, usually with some degree of hair loss, and become much larger in a matter of days.
Hot spots on dogs can be relatively minor and heal quickly. But they do have the potential to cause more serious issues, such as widespread infection or deeper skin ulcerations.
With mild cases, we use listerine! We also have a powder our vet prescribes that we keep on hand. Our bigger, All-American rescue dogs (retriever, German Shepherd, chow mixes) tend to get hot spots more than the pugs so it's a regular thing with them, especially in the summer.
The actual hot spot lesion can range in size. But hot spots are usually red, inflamed, and raw, and they may bleed intermittently.
The area will become moist and painful. It typically spreads due to licking, chewing, and/or scratching.
Hot spots on dogs will usually look different than other skin conditions, such as ringworm or mange, because the skin is very moist and inflamed. For example, ringworm (as well as some parasitic skin infections) will have associated hair loss but are usually drier in appearance compared to hot spots.
Certain breeds are predisposed to skin conditions, including hot spots. Commonly affected breeds include Golden Retrievers, English Bulldogs, and German Shepherds.
Most hot spots on dogs are caused by an underlying condition that either causes itchiness, excessive licking, or excessive moisture. The most common conditions include:
Out of all the possible skin conditions in dogs, hot spots are among the most common. Hot spots can have different underlying causes and treatments based on severity.
Hot spots, also known as acute moist dermatitis, are painful red areas of infected skin that appear to be irritated and are sometimes raised.
Hot spots on dogs can occur anywhere on the body, but they are commonly found on the face, neck, limbs, or hips. The size and appearance of the lesions can vary slightly in each location, but most will look similar regardless of where they are. These spots can appear quickly, usually with some degree of hair loss, and become much larger in a matter of days.
Hot spots on dogs can be relatively minor and heal quickly. But they do have the potential to cause more serious issues, such as widespread infection or deeper skin ulcerations.
With mild cases, we use listerine! We also have a powder our vet prescribes that we keep on hand. Our bigger, All-American rescue dogs (retriever, German Shepherd, chow mixes) tend to get hot spots more than the pugs so it's a regular thing with them, especially in the summer.
The actual hot spot lesion can range in size. But hot spots are usually red, inflamed, and raw, and they may bleed intermittently.
The area will become moist and painful. It typically spreads due to licking, chewing, and/or scratching.
Hot spots on dogs will usually look different than other skin conditions, such as ringworm or mange, because the skin is very moist and inflamed. For example, ringworm (as well as some parasitic skin infections) will have associated hair loss but are usually drier in appearance compared to hot spots.
Certain breeds are predisposed to skin conditions, including hot spots. Commonly affected breeds include Golden Retrievers, English Bulldogs, and German Shepherds.
Most hot spots on dogs are caused by an underlying condition that either causes itchiness, excessive licking, or excessive moisture. The most common conditions include:
- Allergies (flea allergy, food allergy, or seasonal allergies)
- Ear infections
- Excessive moisture from swimming
- Excessive licking due to boredom
- Poor grooming
- Anal gland inflammation
While some hot spots can be treated at home, the underlying cause should always be identified, if possible, to prevent more hot spots from occurring.
Hot spots on dogs can occur anywhere on the body, but they are commonly found on the face, neck, limbs, or hips.
To determine the underlying cause (especially for large or overly infected hot spots on dogs), a veterinary exam is necessary. It’s even more urgent if the affected area is: - Increasing in size
- Consistently bleeding
- You should also seek veterinary attention sooner if you cannot keep your pet from licking or scratching at the hot spot.
- Displaying colored discharge
Depending on the hot spot’s severity, most veterinarians will treat the area with a combination of oral antibiotics, anti-itch medication, and a recovery cone. The area may be clipped and cleaned with antiseptic.
Additional medications (such as flea prevention or allergy medication) may be necessary to treat the underlying cause. By getting your pet veterinary care as soon as possible, you can prevent further infection.Home Remedies for Hot Spots on Dogs
If you aren’t able to get to the vet right away, there are a few things you can do at home to help heal hot spots before your appointment.
Human medications such as Neosporin, hydrocortisone, and Vaseline should NOT be used. Topical creams and ointments tend to cause dogs to lick the area even more, so they should be avoided if possible.
Follow these steps to promote healing of the hot spot: - Trim the area around the hot spot with dog hair clippers (not scissors, which make it easy to accidentally cut your pet’s skin). This allows the affected area to get some air and prevent excess moisture from slowing down the healing process.
- Clean the skin with a mild, water-based antiseptic spray or wipe (like Douxo Chlorhexidine 3% PS pads) or an antibacterial shampoo.
- Apply a veterinary-recommended hot spot treatment spray that is safe if ingested. One example is Vetericyn Plus Antimicrobial Pet Hot Spot Spray.
- Place a recovery cone on your dog to help keep them from biting, licking, or scratching the hot spot.
- Monitor the area for improvement and signs of healing (decreased redness, less moisture, smaller lesion size).
- Contact your veterinarian for an exam to treat the underlying issue, and notify them if the area is not healing or is getting worse.
Demodectic Mange
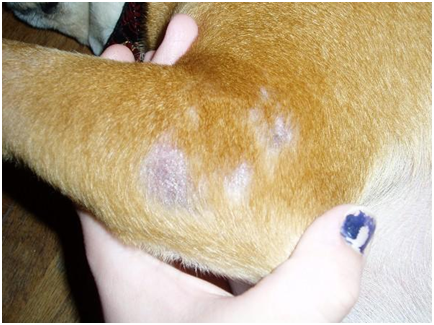
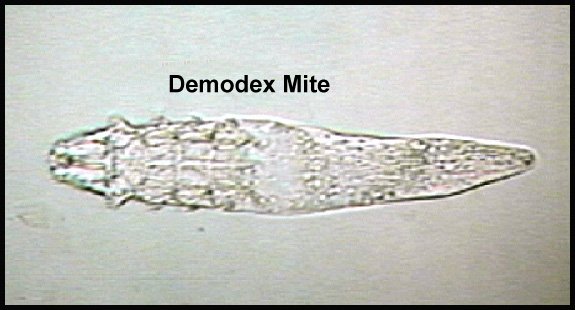
Usually a problem in young Pug puppies, this mange, caused by the Demodex mite, appears as patchy hair loss in 1 or more areas. The skin is sometimes pink and there may be an odor. There can be a secondary bacterial infection associated with this disease which can make the condition itchy. It is diagnosed by a deep skin scraping. It is not thought to be contagious. There are many treatments available. (When we have dealt with this on 2 occasions over the years, we just gave one Bravecto tablet and it eventually cleared up. But it takes time for the fur to grow back, and sometimes it gets worse after the rx before it starts to get better. Brace yourself; your pug might look like a holocaust victim for awhile.) It is thought to “run” in families so dogs that are affected should not be bred, especially if they have more than 1 or 2 small patches as puppies. Demodex can appear in older dogs but they often have compromised immune systems or other diseases as well.
Usually a problem in young Pug puppies, this mange, caused by the Demodex mite, appears as patchy hair loss in 1 or more areas. The skin is sometimes pink and there may be an odor. There can be a secondary bacterial infection associated with this disease which can make the condition itchy. It is diagnosed by a deep skin scraping. It is not thought to be contagious. There are many treatments available. (When we have dealt with this on 2 occasions over the years, we just gave one Bravecto tablet and it eventually cleared up. But it takes time for the fur to grow back, and sometimes it gets worse after the rx before it starts to get better. Brace yourself; your pug might look like a holocaust victim for awhile.) It is thought to “run” in families so dogs that are affected should not be bred, especially if they have more than 1 or 2 small patches as puppies. Demodex can appear in older dogs but they often have compromised immune systems or other diseases as well.
Yeast Infections
If your Pug stinks like dirty feet, is very itchy and has blackened, thickened skin, his problem could be a yeast infection. This problem can often be seen in a dog which had a previous Staph infection and was treated with antibiotics because the drug kills off the bacteria and the yeast takes over. The most commonly seen locations are in the armpits, on the feet, in the groin and on the underside of the neck. When there is a yeast infection in the ears, there is usually a foul odor and excessive light tan or golden wax. Your vet will need to do skin scrapings and ear swabs. There are special anti-yeast medications and shampoos available.
If your Pug stinks like dirty feet, is very itchy and has blackened, thickened skin, his problem could be a yeast infection. This problem can often be seen in a dog which had a previous Staph infection and was treated with antibiotics because the drug kills off the bacteria and the yeast takes over. The most commonly seen locations are in the armpits, on the feet, in the groin and on the underside of the neck. When there is a yeast infection in the ears, there is usually a foul odor and excessive light tan or golden wax. Your vet will need to do skin scrapings and ear swabs. There are special anti-yeast medications and shampoos available.
Staff Infections
Staph is a kind of bacteria that is commonly found on skin. Some dogs will break out in pimples and infected hair follicles if their immune systems are stressed. The lesions can look like hives because they make the hair stick up on the bumps. On non-haired areas, the lesions can look like ringworm – a circular patch with a crusty leading edge and sometimes a dark center. Your vet will usually prescribe oral antibiotics and medicated shampoo.
Staph is a kind of bacteria that is commonly found on skin. Some dogs will break out in pimples and infected hair follicles if their immune systems are stressed. The lesions can look like hives because they make the hair stick up on the bumps. On non-haired areas, the lesions can look like ringworm – a circular patch with a crusty leading edge and sometimes a dark center. Your vet will usually prescribe oral antibiotics and medicated shampoo.
Burns (1st degree, minor burn):
Clip hair from area. Apply strong, lukewarm tea (for its tannic acid content) on a sheet strip compress. Immediately immerse the burn in cool tap water or apply cold, wet compresses. Do this for about 10 minutes or until the pain subsides. Apply petroleum jelly (Vaseline) two to three times daily. Do not apply ointments, toothpaste or butter to the burn, as these may cause an infection. Give tramadol or x as recommended if dog is in pain. Keep him warm if he seems to be in shock.
Clip hair from area. Apply strong, lukewarm tea (for its tannic acid content) on a sheet strip compress. Immediately immerse the burn in cool tap water or apply cold, wet compresses. Do this for about 10 minutes or until the pain subsides. Apply petroleum jelly (Vaseline) two to three times daily. Do not apply ointments, toothpaste or butter to the burn, as these may cause an infection. Give tramadol or x as recommended if dog is in pain. Keep him warm if he seems to be in shock.
Constipation: When your pug isn’t having successful bowel movements, or as frequently as he usually does, or at all, he is probably constipated. The stool (if they do have a bowel movement) will be small, hard, and dry, and it will be painful as your dog struggles to pass it.
Most dogs defecate 1-3 times per day, often after a meal. Normal stool is soft but still holds its form. Constipation is uncommon in dogs, but often easy to treat. It can also be mild or severe. Severe constipation can lead to a condition called obstipation, in which defecation is impossible. Prolonged or repeated obstipation can lead to megacolon. In this condition, the muscles of the colon wall become permanently stretched and can no longer function properly.
Here’s what you need to know about constipation in dogs, from signs and causes to when you can treat it at home and when you need to go to the vet.
SIGNS OF CONSTIPATION
CAUSES OF CONSTIPATION
The number one reason for constipation in dogs is eating things that are indigestible, which become lodged in the colon, preventing feces from advancing. Other reasons for constipation include:
Diet
Pain That Hinders Pooping Neurologic Conditions
When to Go to the Vet for Dog Constipation
If it has not been at least 2 days yet, follow these steps:
Constipation in Puppies
Constipation in puppies is not common, so a straining puppy will more likely have diarrhea.
Newborn puppies need to be manually stimulated by their mother or pet parent to urinate and defecate regularly. If they have structural anomalies in or around the intestinal tract from abnormal development, this can slow down the food or stop it from flowing through the digestive tract.
Large amounts of intestinal parasites can block a puppy’s intestines, as well as any material they may ingest. Puppies are far more sensitive to dehydration and lack of food than adult dogs, so their condition can worsen quickly.
If a puppy has any of the following symptoms, contact your veterinarian immediately:
The best way to prevent constipation in your pug is to treat the underlying causes that your vet identifies.
This may involve thyroid supplementation, surgery to remove strictures or tumors, antibiotics, or pain management, for example. Any medications suspected of contributing to constipation should be changed or discontinued. Follow all instructions from your veterinarian carefully.
Work with your veterinarian to choose a well-balanced, easily digestible diet. A veterinary high-fiber diet or a veterinary low-residue diet (low in fiber and easy to digest) may be recommended.
Medications, including bulking agents, stool softeners, and/or prokinetics, will be prescribed and adjusted over time. Some cases require long-term medication administration.
Here are some other helpful tips for preventing constipation:
Using a daily probiotic helps tremendously. We also often give canned pumpkin (not the pie filling, but pure pumpkin) and every October we cut up and puree lots of pumpkins and freeze. This is the probiotic we use and recommend:
Most dogs defecate 1-3 times per day, often after a meal. Normal stool is soft but still holds its form. Constipation is uncommon in dogs, but often easy to treat. It can also be mild or severe. Severe constipation can lead to a condition called obstipation, in which defecation is impossible. Prolonged or repeated obstipation can lead to megacolon. In this condition, the muscles of the colon wall become permanently stretched and can no longer function properly.
Here’s what you need to know about constipation in dogs, from signs and causes to when you can treat it at home and when you need to go to the vet.
SIGNS OF CONSTIPATION
- Smaller, drier feces that are more difficult for the colon to move forward, and your pug becomes constipated.
- Seeing your pug straining to defecate, but this can be easily confused with other problems such as diarrhea and having trouble peeing. (If you see that your dog can’t urinate, call an emergency vet right away, as this is a medical emergency.)
- As constipation becomes more severe, your dog may become lethargic, stop eating, or begin vomiting. If you see any of these signs, call an emergency vet right away.
- Scooting (dragging their bottom across the ground) due to discomfort
- Swelling around the anus
- Circling or pacing between episodes of straining
- Vocalizing while trying to poop
- Less frequent bowel movements
- Passing small, hard pieces of stool that are sometimes foul-smelling and/or left in odd places (such as corners and basements)
- Hunched appearance
- Sensitive stomach (your dog won’t want you to touch it)
- Passing a small amount of liquid with mucus and/or blood (caused by excessive straining)
CAUSES OF CONSTIPATION
The number one reason for constipation in dogs is eating things that are indigestible, which become lodged in the colon, preventing feces from advancing. Other reasons for constipation include:
Diet
- Indigestible items (e.g., large amounts of fur, bones, litter, etc.)
- Diet change
- Low-fiber diet
- Stress from boarding, traveling, new person or pet in home, new schedule for family members
- Getting less exercise (e.g., recent hospitalization, change in mobility)
Pain That Hinders Pooping Neurologic Conditions
- Nerve damage
- Tumors
- Disc disease
- Prostate enlargement (e.g., inflammation, tumor)
- Previous pelvic fracture
- Intestinal stricture
- Enlarged abdominal lymph nodes
- Tumors of the rectum or anus
- Hypothyroidism
- Chronic kidney disease
- Calcium and electrolyte abnormalities
- Opioids
- Antihistamines
- Diuretics
- Sucralfate (for ulcers)
When to Go to the Vet for Dog Constipation
- Lethargy, decreased appetite, vocalizing, and vomiting are all signs of more severe cases. If you see these, call your vet and don’t try to manage the condition at home.
- If your pug has not had a bowel movement in 48-72 hours, it’s also time to call the vet.
If it has not been at least 2 days yet, follow these steps:
- When you see your pug straining, check to make sure that he is able to urinate. It can be easy to mistake straining to urinate and straining to defecate. Not being able to pee is a medical emergency in dogs that should be checked out right away.
- Next, if your dog is able to poop, check the consistency of the stool to see if there is evidence of diarrhea. If you see diarrhea or a small amount of liquid with mucus or blood, contact your vet.
- Look at your dog’s rear end. Check for the following:
- Redness, swelling, and/or open sores (signs of abscesses). If you see any of these, go to the vet right away.
- Fecal matter or hair that may be matted over the anus. If you see this, soak the area well with warm water, and gently remove the feces. If possible, trim the fur to prevent further matting, and monitor for further signs of constipation or diarrhea.
- Try taking your dog on a long walk or more frequent walks. Exercise can stimulate the colon and may relieve constipation.
- To increase hydration, try switching to canned food or adding water to kibble.
- You can also add 100% canned pumpkin (not pie filling with other ingredients) or Metamucil to each meal. Canned pumpkin does not have as much relevant fiber as Metamucil or bran, but it is more readily available and can be sufficient for milder cases.
- Canned pumpkin: Give 1-4 tablespoons per meal depending on the size of your dog. (1 TB for small breeds, 2-3 TB for medium breeds, and 4 TB for large breeds)
- Metamucil: Contact your vet for the right amount for your dog.
- DO NOT give mineral oil or white petrolatum to your dog. These unflavored items can be easily inhaled, leading to fatal aspiration pneumonia.
- DO NOT use any over-the-counter enemas, unless specifically instructed by your veterinarian. Many common human enemas are toxic to dogs.
- Giving your dog coconut oil or olive oil is also not recommended. Inappropriate amounts can lead to pancreatitis, bloat, vomiting, or diarrhea. Talk to your veterinarian first.
Constipation in Puppies
Constipation in puppies is not common, so a straining puppy will more likely have diarrhea.
Newborn puppies need to be manually stimulated by their mother or pet parent to urinate and defecate regularly. If they have structural anomalies in or around the intestinal tract from abnormal development, this can slow down the food or stop it from flowing through the digestive tract.
Large amounts of intestinal parasites can block a puppy’s intestines, as well as any material they may ingest. Puppies are far more sensitive to dehydration and lack of food than adult dogs, so their condition can worsen quickly.
If a puppy has any of the following symptoms, contact your veterinarian immediately:
- Has not passed any stool in 24 hours
- Is not eating
- Is vomiting or retching
- Appears to be in pain
- Is lethargic
- Has a distended belly
The best way to prevent constipation in your pug is to treat the underlying causes that your vet identifies.
This may involve thyroid supplementation, surgery to remove strictures or tumors, antibiotics, or pain management, for example. Any medications suspected of contributing to constipation should be changed or discontinued. Follow all instructions from your veterinarian carefully.
Work with your veterinarian to choose a well-balanced, easily digestible diet. A veterinary high-fiber diet or a veterinary low-residue diet (low in fiber and easy to digest) may be recommended.
Medications, including bulking agents, stool softeners, and/or prokinetics, will be prescribed and adjusted over time. Some cases require long-term medication administration.
Here are some other helpful tips for preventing constipation:
- Closely monitor the frequency and consistency of your pug’s stool.
- Ensure that your pug gets plenty of exercise daily.
- Avoid dehydration by offering multiple sources of freshwater, or feed canned food to increase water intake.
- Groom your dog regularly, keeping the fur around the anus short.
- Avoid giving your pug bones or other undigestible items, and prohibit access to things that may cause constipation, including litter or clothing.
- Other management options that may foster regular bowel movements and a healthy intestinal tract include a daily probiotic and acupuncture.
Using a daily probiotic helps tremendously. We also often give canned pumpkin (not the pie filling, but pure pumpkin) and every October we cut up and puree lots of pumpkins and freeze. This is the probiotic we use and recommend:
Diarrhea - two major categories: large-bowel and small-bowel diarrhea. Large-Bowel Diarrhea (or diarrhea arising from the large intestine or colon), is characterized by:
Small-Bowel Diarrhea (or diarrhea arising from the small intestine), is characterized by:
Chronic Diarrhea Chronic diarrhea is persistent despite initial treatment or is recurrent in nature. Causes include (but are not limited to):
If your pet is continuously exposed to a diet that they are sensitive to, this can also cause chronic intermittent diarrhea.
Some dog and cat foods that are marketed as healthier for your pet can also be high in fat and protein. Grain-free diets remove healthy fiber content from the dog food, which can be very rough on a sensitive system.
It is important to look for balance in a diet and that it comes from a reputable company that is doing their homework when it comes to their formulations.
Diarrhea With Vomiting - When diarrhea occurs with vomiting, a new section of the gastrointestinal tract has entered the picture. Gastroenteritis is the group term for inflammation of both the stomach and the upper GI tract.
Sometimes a high-fat treat, even a small one, can trigger pancreatitis—a condition wherein the pancreas, which produces digestive enzymes, among other things, becomes inflamed. This condition can cause acute vomiting and diarrhea as well as abdominal pain. In very severe cases, pancreatitis can even be fatal. Vomit that contains blood can look red, brown, or black. Unlike a small amount of blood in the stool, any amount of blood in vomit is concerning and should result in a trip to the vet right away.
What Does the Color of Your Dog’s Diarrhea Mean? The color of your pet’s bowel movement is most often impacted by what they are eating. Simply put, lighter colored foods will result in a lighter colored poop. There are a few color indicators that are important to note when talking to your vet.
Yellow diarrhea is most typically caused when a pet parent has started feeding a bland diet, such as chicken and rice. The chicken and rice are white, and when they mix with yellow bile in the gastrointestinal tract, it comes out as yellow stools.
Bloody diarrhea or hematochezia is caused when there is large bowel diarrhea or colitis. This occurs when small blood vessels in the lower part of the GI tract break open and bleed a bit into the stool. A small amount of blood is not overly concerning, but if the stool is primarily blood, your pet should be taken to the vet right away.
Black diarrhea or melena is caused when blood is being digested before it is passed. This stool looks like newborn baby poop and can have a black or greenish color. Melena can be seen with conditions such as bleeding ulcers or foreign bodies.
- Increased frequency
- Small volumes of stool
- Straining to defecate
- Red blood in the stool as well as mucous
Small-Bowel Diarrhea (or diarrhea arising from the small intestine), is characterized by:
- Large, goopy poops produced at normal frequency
- Stool is often fatty and frothy
- Stool rarely has red blood or mucous
- There is typically no straining involved
- The job of the small intestine is absorption of nutrients. When there is inflammation or dysfunction, there can be a lack of absorption, resulting in fatty stools.
- Weight loss
- Poor hair coat
- Ravenous appetite
Chronic Diarrhea Chronic diarrhea is persistent despite initial treatment or is recurrent in nature. Causes include (but are not limited to):
- Parasites such as whipworms
- Inflammatory bowel disease
- Exocrine pancreatic insufficiency
- Hyperthyroidism or other metabolic condition
- Cancer
- Dysbiosis
If your pet is continuously exposed to a diet that they are sensitive to, this can also cause chronic intermittent diarrhea.
Some dog and cat foods that are marketed as healthier for your pet can also be high in fat and protein. Grain-free diets remove healthy fiber content from the dog food, which can be very rough on a sensitive system.
It is important to look for balance in a diet and that it comes from a reputable company that is doing their homework when it comes to their formulations.
Diarrhea With Vomiting - When diarrhea occurs with vomiting, a new section of the gastrointestinal tract has entered the picture. Gastroenteritis is the group term for inflammation of both the stomach and the upper GI tract.
Sometimes a high-fat treat, even a small one, can trigger pancreatitis—a condition wherein the pancreas, which produces digestive enzymes, among other things, becomes inflamed. This condition can cause acute vomiting and diarrhea as well as abdominal pain. In very severe cases, pancreatitis can even be fatal. Vomit that contains blood can look red, brown, or black. Unlike a small amount of blood in the stool, any amount of blood in vomit is concerning and should result in a trip to the vet right away.
What Does the Color of Your Dog’s Diarrhea Mean? The color of your pet’s bowel movement is most often impacted by what they are eating. Simply put, lighter colored foods will result in a lighter colored poop. There are a few color indicators that are important to note when talking to your vet.
Yellow diarrhea is most typically caused when a pet parent has started feeding a bland diet, such as chicken and rice. The chicken and rice are white, and when they mix with yellow bile in the gastrointestinal tract, it comes out as yellow stools.
Bloody diarrhea or hematochezia is caused when there is large bowel diarrhea or colitis. This occurs when small blood vessels in the lower part of the GI tract break open and bleed a bit into the stool. A small amount of blood is not overly concerning, but if the stool is primarily blood, your pet should be taken to the vet right away.
Black diarrhea or melena is caused when blood is being digested before it is passed. This stool looks like newborn baby poop and can have a black or greenish color. Melena can be seen with conditions such as bleeding ulcers or foreign bodies.
Treating Dog Diarrhea At Home
You should never use your own human medications on your pets. Only administer medications as prescribed by your veterinarian.
You should never use your own human medications on your pets. Only administer medications as prescribed by your veterinarian.
- Antibiotics can make diarrhea worse
- In our experience, Pepto Bismol just results in pink vomit
- Imodium works by paralyzing the gastrointestinal tract. This can be a problem for pets that eat things they aren’t supposed to (such as toxins or foreign objects) or have parasites that need to be moved through.
- Feed small, frequent meals that help heal the GI tract but do not overwhelm it.
- In the case of stress-induced diarrhea, starting a fiber supplement a few days prior to the stressful event can help prevent the diarrhea from starting. Psyllium fiber can be purchased over the counter in products like Metamucil.
Pneumonia
Pneumonia is irritation and inflammation within the lungs that results in the buildup of fluid within the air sacs. This compromises the normal exchange of oxygen and carbon dioxide within the lungs, resulting in difficult breathing. Pneumonia can be caused by various reasons, including:
Symptoms of Dog PneumoniaPneumonia causes many symptoms, ranging from mild to severe. Most common symptoms include:
Causes of Dog Pneumonia
Pneumonia has many origins, and often a dog can have multiple types of pneumonia at once. This happens most often with secondary bacterial infections.
Aspiration Pneumonia
Most pug owners are quite familiar with AP, especially pug breeders who deal with newborn puppies aspirating milk while nursing. Aspiration pneumonia occurs when a dog breathes in substances like food or vomit. It is one of the more common types of pneumonia. The inhaled food material physically blocks air spaces and sets off an inflammatory cascade within the lungs. Stomach acids can also directly damage lung cells. All these factors combined create a perfect environment for a secondary bacterial infection. Some animals are at a higher risk for developing aspiration pneumonia due to factors such as:
Bacterial Pneumonia
Bacterial pneumonia is common in dogs. Bacteria typically enters the lungs through aspiration or inhalation, but rarely spreads throughout the bloodstream. Most healthy adult animals do not acquire primary bacterial pneumonia. Puppies, seniors and immunocompromised dogs are more susceptible to bacterial pneumonia. Typically, this type of pneumonia is a secondary condition, or works in conjunction of a bigger respiratory issue involving multiple bacteria and viruses. Common bacteria found in dogs with pneumonia include:
Inhalation PneumoniaInhalation pneumonia may occur because of breathing noxious fumes or gases, including chemicals and smoke. Toxic particles interfere with the body’s ability to process oxygen normally, while also affecting the normal mucus and clearance within the lungs.
How Veterinarians Diagnose Dog PneumoniaVeterinarians use many diagnostics tests to diagnose pneumonia. Typically, they will start with listening to the lungs with a stethoscope. Fluid in the chest may sound like crackles, wheezes and pops. Occasionally, the lungs are only quieter than normal. This symptom, combined with coughing or difficulty breathing, may lead a veterinarian to recommend additional diagnostic tests.
Radiograph
Veterinarians use radiographs, or X-rays of the chest to diagnose pneumonia, and a specialized 3-view X-ray to help determine its severity. Fluid and inflammation look much different from air on X-rays, with gray, patchy or a hazy pattern. Pneumonia can affect one lung lobe or multiple lobes. Lungs can even collapse as fluid replaces the entirety of the air sacs.
Blood Chemistry and Complete Blood Count (CBC)
The complete blood count, or CBC, may show signs of inflammation and infection. The blood chemistry may show signs of sepsis in severe cases, as well as predisposing factors or reasons for vomiting.
Pulse Oximetry and Blood-Gas Analysis
Veterinarians use pulse oximetry and blood gas analysis to determine if the patient is receiving sufficient oxygen, and to confirm the presence of respiratory dysfunction. This is also an integral part of the follow-up and treatment monitoring process. Pulse oximetry, a small infrared light, is a non-invasive test that reads how much oxygen is present in the capillaries. Blood-gas analysis requires a special catheter to collect blood to analyze for oxygen, carbon dioxide and pH, among other things.
Culture and Cytology
Dogs with pneumonia may undergo procedures such as transtracheal washes, bronchoalveolar lavage and a bronchoscopy to obtain fluid samples from within the lungs. These procedures require special instruments designed to explore the respiratory tract and obtain the purest sample. Veterinarians can evaluate the samples under a microscope and look for cells and pathogenic organisms. Once cultured, veterinarians identify specific bacterial pathogens and then prescribe the best antibiotic therapy.
Other Tests
Veterinarians can use advanced imaging, such as MRI or CT to fully assess the extent of pneumonia and other risk factors. They may use other tests for infectious agents and parasites, including PCR, serology, etc. Blood cultures are rarely used, as a local culture typically yields good results.
Treatment
Therapy depends on the type of pneumonia and underlying pathology, or other illnesses. The severity of the disease will also dictate the intensity of treatment. Mild cases of pneumonia can be managed on an outpatient basis with medications, rest and home care. Moderate to severe cases require hospitalization - often at emergency facilities - with 24/7 nursing care and special equipment.
Antibiotics
Veterinarians prescribe antibiotics to dogs with primary or secondary bacterial pneumonia. Most common antibiotics include Doxycycline, Fluoroquinolone and Amoxicillin-clavulanic Acid. Treatment length is typically long-term, sometimes more than a month. Frequent rechecks help determine how long the antibiotics must be taken.
Oxygen Therapy
For animals who cannot oxygenate sufficiently on room-air, they are placed on supplemental oxygen. This may be a nasal or face mask, but veterinarians most commonly utilize an oxygen cage. An oxygen cage is an enclosed environment where the oxygen can be manipulated from room air (20 percent oxygen) to 100 percent oxygen. This is typically the least stressful way to supply oxygen to dogs in respiratory distress, and indicates the dog’s level of illness.
Fluid Therapy
Dogs with pneumonia are typically dehydrated and require an intravenous catheter and fluid therapy to rehydrate. Dehydration impairs respiratory clearance and function, so this is especially important in cases of pneumonia.
Nebulization and Coupage
Nebulizers create a fine mist and allow a localized increase in humidity, like the moist environment of a bathroom when the shower is on. Most nebulizers use saline to increase hydration of the airway but can also add antibiotics. After a nebulization treatment, dogs with pneumonia may have coupage performed, which is a gentle yet firm tap around the chest. Together, nebulization and coupage help break apart and clear mucus and other cells trapped in the airways.
Ventilation
Severe cases of pneumonia require full sedation and a ventilator to breathe. This is typically done if a dog does not respond to initial oxygen therapy or is minimally unresponsive. This typically happens only in an intensive care unit.
Recovery and Management of Dog PneumoniaX-rays are typically taken every two to five days during the acute phase, and then every one to two weeks (as needed) until complete resolution. X-rays should be monitored for recurrence every few months after full resolution. A veterinarian will want to recheck an exam as well as bloodwork within the first two weeks after an episode of pneumonia.
Most veterinarians recommend the continuation of treatment for at least a week after resolution of clinical signs – both patient symptoms and X-ray evidence.
Veterinarians do not typically recommend cough suppressants for dogs recovering from pneumonia. Coughing is the body’s natural way to remove the infection and fluid within the airways.
Is dog pneumonia contagious?Some forms of canine pneumonia, such as viral or bacterial components, are contagious to other dogs.
What is the survival rate for dogs with pneumonia?The prognosis for canine pneumonia is typically very good, with early and aggressive veterinary treatment. Studies show approximately 77 to 94 percent of patients with bacterial pneumonia survive to discharge.
How do I know if my dog has pneumonia?Dogs with pneumonia are typically very sick, lethargic and act abnormally. If your pet is having difficulty or changes in breathing, contact your veterinarian or go directly to an emergency hospital for treatment.
Pneumonia is irritation and inflammation within the lungs that results in the buildup of fluid within the air sacs. This compromises the normal exchange of oxygen and carbon dioxide within the lungs, resulting in difficult breathing. Pneumonia can be caused by various reasons, including:
- Bacteria
- Viruses
- Fungal organisms
- Parasites
- Immune-mediated
- Inhalation of stomach contents, food, chemicals, fluids, foreign materials
- Inhalation of chemicals, smoke
Symptoms of Dog PneumoniaPneumonia causes many symptoms, ranging from mild to severe. Most common symptoms include:
- Cough
- Labored breathing
- Nasal discharge
- Wheezing
- Fever
- Lethargy
- Respiratory distress
- Blue gums, in severe cases
Causes of Dog Pneumonia
Pneumonia has many origins, and often a dog can have multiple types of pneumonia at once. This happens most often with secondary bacterial infections.
Aspiration Pneumonia
Most pug owners are quite familiar with AP, especially pug breeders who deal with newborn puppies aspirating milk while nursing. Aspiration pneumonia occurs when a dog breathes in substances like food or vomit. It is one of the more common types of pneumonia. The inhaled food material physically blocks air spaces and sets off an inflammatory cascade within the lungs. Stomach acids can also directly damage lung cells. All these factors combined create a perfect environment for a secondary bacterial infection. Some animals are at a higher risk for developing aspiration pneumonia due to factors such as:
- Laryngeal impairment
- Under sedation or anesthesia
- Neurologic disorders
- Medically required force-feeding
- Being prone to vomiting or regurgitation
- Brachycephalic breeds (Pugs, Bulldogs, Boston Terriers, etc.)
Bacterial Pneumonia
Bacterial pneumonia is common in dogs. Bacteria typically enters the lungs through aspiration or inhalation, but rarely spreads throughout the bloodstream. Most healthy adult animals do not acquire primary bacterial pneumonia. Puppies, seniors and immunocompromised dogs are more susceptible to bacterial pneumonia. Typically, this type of pneumonia is a secondary condition, or works in conjunction of a bigger respiratory issue involving multiple bacteria and viruses. Common bacteria found in dogs with pneumonia include:
- Bordetella
- Mycoplasma
- Yersinia
- Streptococcus
- E. coli
- Klebsiella
- Pseudomonas
- Enterococcus
- Pasteurella
- Bacillus
- Fusobacterium
- Viral or fungal pneumonia
- Immunosuppression from drugs or other illnesses
- Cancer
- Prolonged surgery
- Airway obstruction or anatomic abnormalities
- Vomiting and subsequent aspiration
- Metabolic disorders
- Abnormal mentation, such as seizures
- Inhaled foreign bodies
- Damaged cells in the lungs secondary to smoke or chemical inhalation, and drowning
- Sepsis
- Canine influenza
- Canine distemper
- Canine adenovirus-2
- Canine herpesvirus
- Canine parainfluenza virus
- Blastomyces
- Histoplasma
- Neospora
- Toxoplasma
Inhalation PneumoniaInhalation pneumonia may occur because of breathing noxious fumes or gases, including chemicals and smoke. Toxic particles interfere with the body’s ability to process oxygen normally, while also affecting the normal mucus and clearance within the lungs.
How Veterinarians Diagnose Dog PneumoniaVeterinarians use many diagnostics tests to diagnose pneumonia. Typically, they will start with listening to the lungs with a stethoscope. Fluid in the chest may sound like crackles, wheezes and pops. Occasionally, the lungs are only quieter than normal. This symptom, combined with coughing or difficulty breathing, may lead a veterinarian to recommend additional diagnostic tests.
Radiograph
Veterinarians use radiographs, or X-rays of the chest to diagnose pneumonia, and a specialized 3-view X-ray to help determine its severity. Fluid and inflammation look much different from air on X-rays, with gray, patchy or a hazy pattern. Pneumonia can affect one lung lobe or multiple lobes. Lungs can even collapse as fluid replaces the entirety of the air sacs.
Blood Chemistry and Complete Blood Count (CBC)
The complete blood count, or CBC, may show signs of inflammation and infection. The blood chemistry may show signs of sepsis in severe cases, as well as predisposing factors or reasons for vomiting.
Pulse Oximetry and Blood-Gas Analysis
Veterinarians use pulse oximetry and blood gas analysis to determine if the patient is receiving sufficient oxygen, and to confirm the presence of respiratory dysfunction. This is also an integral part of the follow-up and treatment monitoring process. Pulse oximetry, a small infrared light, is a non-invasive test that reads how much oxygen is present in the capillaries. Blood-gas analysis requires a special catheter to collect blood to analyze for oxygen, carbon dioxide and pH, among other things.
Culture and Cytology
Dogs with pneumonia may undergo procedures such as transtracheal washes, bronchoalveolar lavage and a bronchoscopy to obtain fluid samples from within the lungs. These procedures require special instruments designed to explore the respiratory tract and obtain the purest sample. Veterinarians can evaluate the samples under a microscope and look for cells and pathogenic organisms. Once cultured, veterinarians identify specific bacterial pathogens and then prescribe the best antibiotic therapy.
Other Tests
Veterinarians can use advanced imaging, such as MRI or CT to fully assess the extent of pneumonia and other risk factors. They may use other tests for infectious agents and parasites, including PCR, serology, etc. Blood cultures are rarely used, as a local culture typically yields good results.
Treatment
Therapy depends on the type of pneumonia and underlying pathology, or other illnesses. The severity of the disease will also dictate the intensity of treatment. Mild cases of pneumonia can be managed on an outpatient basis with medications, rest and home care. Moderate to severe cases require hospitalization - often at emergency facilities - with 24/7 nursing care and special equipment.
Antibiotics
Veterinarians prescribe antibiotics to dogs with primary or secondary bacterial pneumonia. Most common antibiotics include Doxycycline, Fluoroquinolone and Amoxicillin-clavulanic Acid. Treatment length is typically long-term, sometimes more than a month. Frequent rechecks help determine how long the antibiotics must be taken.
Oxygen Therapy
For animals who cannot oxygenate sufficiently on room-air, they are placed on supplemental oxygen. This may be a nasal or face mask, but veterinarians most commonly utilize an oxygen cage. An oxygen cage is an enclosed environment where the oxygen can be manipulated from room air (20 percent oxygen) to 100 percent oxygen. This is typically the least stressful way to supply oxygen to dogs in respiratory distress, and indicates the dog’s level of illness.
Fluid Therapy
Dogs with pneumonia are typically dehydrated and require an intravenous catheter and fluid therapy to rehydrate. Dehydration impairs respiratory clearance and function, so this is especially important in cases of pneumonia.
Nebulization and Coupage
Nebulizers create a fine mist and allow a localized increase in humidity, like the moist environment of a bathroom when the shower is on. Most nebulizers use saline to increase hydration of the airway but can also add antibiotics. After a nebulization treatment, dogs with pneumonia may have coupage performed, which is a gentle yet firm tap around the chest. Together, nebulization and coupage help break apart and clear mucus and other cells trapped in the airways.
Ventilation
Severe cases of pneumonia require full sedation and a ventilator to breathe. This is typically done if a dog does not respond to initial oxygen therapy or is minimally unresponsive. This typically happens only in an intensive care unit.
Recovery and Management of Dog PneumoniaX-rays are typically taken every two to five days during the acute phase, and then every one to two weeks (as needed) until complete resolution. X-rays should be monitored for recurrence every few months after full resolution. A veterinarian will want to recheck an exam as well as bloodwork within the first two weeks after an episode of pneumonia.
Most veterinarians recommend the continuation of treatment for at least a week after resolution of clinical signs – both patient symptoms and X-ray evidence.
Veterinarians do not typically recommend cough suppressants for dogs recovering from pneumonia. Coughing is the body’s natural way to remove the infection and fluid within the airways.
Is dog pneumonia contagious?Some forms of canine pneumonia, such as viral or bacterial components, are contagious to other dogs.
What is the survival rate for dogs with pneumonia?The prognosis for canine pneumonia is typically very good, with early and aggressive veterinary treatment. Studies show approximately 77 to 94 percent of patients with bacterial pneumonia survive to discharge.
How do I know if my dog has pneumonia?Dogs with pneumonia are typically very sick, lethargic and act abnormally. If your pet is having difficulty or changes in breathing, contact your veterinarian or go directly to an emergency hospital for treatment.
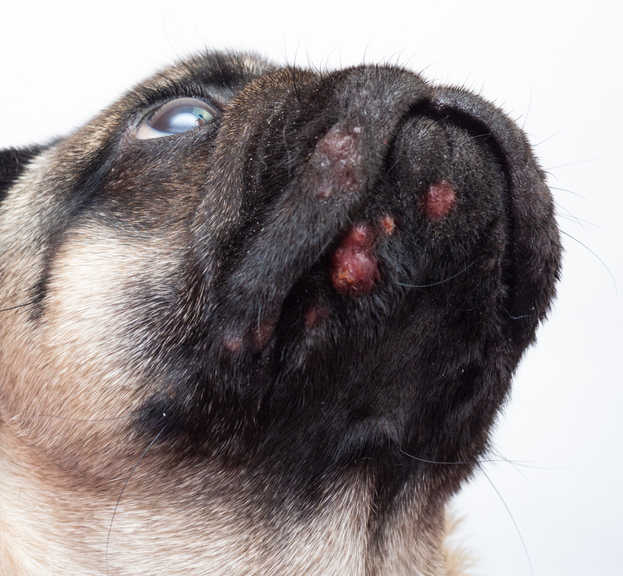
Dog acne is inflammation of the lips and the skin of the muzzle, which can appear as red bumps or pimples on the skin. Acne may begin as folliculitis, which is when short hairs push below the skin’s surface and become inflamed. Acne may also occur due to furunculosis, which is when the hair follicle under the skin (also known as muzzle folliculitis and furunculosis) becomes painful, infected, and inflamed, often filled with pus. This occurs when short hairs on the surface of the skin break and are pushed below the skin surface in the follicle. In both these cases, there is trauma to the tissues, and it can create a chronic condition in which secondary bacterial or fungal infections can complicate the process.
This condition is fairly common in young pugs and other short, coated breeds of dogs.
Symptoms
Dog acne most commonly appears on the bottom of the chin, skin around the mouth, and lower lips. It can look like red bumps, hairless areas, and swelling of the muzzle. As the condition progresses, the bumps can become infected, grow, ooze, or drain fluid.
Causes
Although the cause of dog acne is often unknown, possible factors include:
Dog acne is unique in that typically the only area of the dog affected is the muzzle.
In many cases, the cause of acne is unknown. Some possible causes are localized trauma from rough play or rubbing face on carpet or on rough surfaces. Some pets itch and rub from underlying skin allergies (that affect many parts of the body), and this can complicate or cause the initial acne flare. Not all dogs of the short haired breeds develop chin acne, so it’s likely genetics and environmental causes play a role in this condition.
How Veterinarians Diagnose Dog AcneIt is important to schedule a visit with your veterinarian if you believe your dog has developed acne and is exhibiting any of the above symptoms.
Your veterinarian will want to rule out other conditions, such as:
Typically, your veterinarian will do a thorough examination and ask for history regarding diet, treats, supplements, and home environment (your vet may ask about the types of dishes used for pets or whether other pets are in the home). Some pets can have a contact reaction to plastic bowls. Also, it is possible that contamination of bacteria or yeast can hide in micro scratches on plastic dishes.
Your vet may also take skin samples to look for secondary bacteria, yeast, or Demodex mites and possibly order a dermatophyte fungal culture. A bacterial culture may be taken if the acne shows signs of draining to identify the type of bacteria.
In rare cases, a biopsy may be performed to check deep disease, unusual lesions, or cases not responding to therapy.
Treatment of Dog AcneTreatment of dog acne can include medication, dietary changes, and behavioral therapy.
Your veterinarian may prescribe topical or oral medications to reduce inflammation and fight any bacterial infection, if necessary. Medications can include:
If your vet finds that your dog has an underlying allergy, they may suggest diet therapy, supplements, and allergy medications (prescription or over-the-counter).
Recovery and Management of Dog Acne
Most dogs with acne recover with proper treatment but do require management, which may include preventing recurring trauma, using topical medications during flare ups, and long-term allergy management if necessary. Some severe cases can result in scarring and can be prone to lesion recurrence.
FAQs
What can I do at home to help my dog's acne?
Behavioral modification to limit contact with rough surfaces or rough play can help limit hair breakage. Keeping the chin area clean and dry can help prevent secondary infections.
Will dog acne go away on its own?
Because the follicle becomes inflamed when the broken hair is pushed deep under the skin, dog chin acne usually requires some form of treatment. The treatment may be mild to significant depending on the individual case. Some dogs with a deep skin infection (pyoderma) may require several months on medications.
Is dog acne contagious?
Most often dog acne is not contagious. If there is a secondary bacterial or fungal infection, the chance of spreading the infection is minimal.
Symptoms
Dog acne most commonly appears on the bottom of the chin, skin around the mouth, and lower lips. It can look like red bumps, hairless areas, and swelling of the muzzle. As the condition progresses, the bumps can become infected, grow, ooze, or drain fluid.
Causes
Although the cause of dog acne is often unknown, possible factors include:
- Skin damage from rough play or rubbing the face on a rough surface
- Itching and rubbing triggered by an underlying skin allergy
- Age (most dogs with chin acne are between 6 months and a year old)
- Short hair breeds, such as Boxer, Doberman Pinscher, English Bulldog, Great Dane, Weimaraner, English Mastiff, Rottweiler, and German Short Haired Pointer
Dog acne is unique in that typically the only area of the dog affected is the muzzle.
In many cases, the cause of acne is unknown. Some possible causes are localized trauma from rough play or rubbing face on carpet or on rough surfaces. Some pets itch and rub from underlying skin allergies (that affect many parts of the body), and this can complicate or cause the initial acne flare. Not all dogs of the short haired breeds develop chin acne, so it’s likely genetics and environmental causes play a role in this condition.
How Veterinarians Diagnose Dog AcneIt is important to schedule a visit with your veterinarian if you believe your dog has developed acne and is exhibiting any of the above symptoms.
Your veterinarian will want to rule out other conditions, such as:
- Demodicosis: A type of mange that is typically diagnosed through an examine of skin scrapings under a microscope.
- Ringworm: In its early stages this fungus resembles acne, so your veterinarian will pluck several hairs for a culture. It typically takes 10 to 14 days to determine whether there is a fungal infection.
- Puppy Strangles: A skin disorder that appears in puppies and can resemble acne.
Typically, your veterinarian will do a thorough examination and ask for history regarding diet, treats, supplements, and home environment (your vet may ask about the types of dishes used for pets or whether other pets are in the home). Some pets can have a contact reaction to plastic bowls. Also, it is possible that contamination of bacteria or yeast can hide in micro scratches on plastic dishes.
Your vet may also take skin samples to look for secondary bacteria, yeast, or Demodex mites and possibly order a dermatophyte fungal culture. A bacterial culture may be taken if the acne shows signs of draining to identify the type of bacteria.
In rare cases, a biopsy may be performed to check deep disease, unusual lesions, or cases not responding to therapy.
Treatment of Dog AcneTreatment of dog acne can include medication, dietary changes, and behavioral therapy.
Your veterinarian may prescribe topical or oral medications to reduce inflammation and fight any bacterial infection, if necessary. Medications can include:
- Anti-inflammatories
- Antibiotics
- Antifungals
If your vet finds that your dog has an underlying allergy, they may suggest diet therapy, supplements, and allergy medications (prescription or over-the-counter).
Recovery and Management of Dog Acne
Most dogs with acne recover with proper treatment but do require management, which may include preventing recurring trauma, using topical medications during flare ups, and long-term allergy management if necessary. Some severe cases can result in scarring and can be prone to lesion recurrence.
FAQs
What can I do at home to help my dog's acne?
Behavioral modification to limit contact with rough surfaces or rough play can help limit hair breakage. Keeping the chin area clean and dry can help prevent secondary infections.
Will dog acne go away on its own?
Because the follicle becomes inflamed when the broken hair is pushed deep under the skin, dog chin acne usually requires some form of treatment. The treatment may be mild to significant depending on the individual case. Some dogs with a deep skin infection (pyoderma) may require several months on medications.
Is dog acne contagious?
Most often dog acne is not contagious. If there is a secondary bacterial or fungal infection, the chance of spreading the infection is minimal.
EAR INFECTIONS
A healthy dog ear is clean and dry. It’s normal for small amounts of microscopic bacteria and yeast to live in a dog's outer ear canal, but when a buildup of debris occurs—or the normal, healthy ear canal is compromised—bacteria and yeast can overgrow and cause an infection.
Ear infections are one of the most common type of infections in dogs and typically affect the outer ear (otitis externa). Common clinical signs include head shaking, scratching at the ears, ear odor, and visible debris in the ear.
Pugs are especially prone to skin allergies and ear infections. These problems can start to show up as early as one year of age.
Since Pugs have narrow ear canals and deep folds in the skin around their face, they can collect debris and bacteria more easily. It’s important to clean and dry the skin folds around the face daily, and clean the ears at least weekly, to help prevent inflammation from forming. Regular cleaning also allows you to check the ears and skin to identify inflammation and seek care early.
Skin allergies are not curable, but seeking medications from a veterinarian and doing preventive bathing and ear cleaning to prevent infections caused by allergies will help to keep your Pug comfortable and happy.
SYMPTOMS
A healthy dog ear is clean and dry. It’s normal for small amounts of microscopic bacteria and yeast to live in a dog's outer ear canal, but when a buildup of debris occurs—or the normal, healthy ear canal is compromised—bacteria and yeast can overgrow and cause an infection.
Ear infections are one of the most common type of infections in dogs and typically affect the outer ear (otitis externa). Common clinical signs include head shaking, scratching at the ears, ear odor, and visible debris in the ear.
Pugs are especially prone to skin allergies and ear infections. These problems can start to show up as early as one year of age.
Since Pugs have narrow ear canals and deep folds in the skin around their face, they can collect debris and bacteria more easily. It’s important to clean and dry the skin folds around the face daily, and clean the ears at least weekly, to help prevent inflammation from forming. Regular cleaning also allows you to check the ears and skin to identify inflammation and seek care early.
Skin allergies are not curable, but seeking medications from a veterinarian and doing preventive bathing and ear cleaning to prevent infections caused by allergies will help to keep your Pug comfortable and happy.
SYMPTOMS
- Redness
- Odor (a yeasty, corn chip-like smell)
- Itching/scratching at ears
- Pain
- Shaking of the head
- Head tilt
- Discharge
- Scabs or crusting
- Possibly hearing loss or balance issues
- Rarely, a dog ear infection may affect a dog's appetite.
CAUSES
Often, an underlying problem leads to the inability of the normal protective barrier of a dog’s ear to work properly. Once the ear becomes moist or inflamed, it's easy for bacteria or yeast to overgrow and cause infection in a pup.
These issues can make the ear canal vulnerable to a bacterial infection and/or a yeast infection.
When a dog is in pain and scratching and shaking excessively, an aural hematoma can develop. This is seen in the pinna or earflap, where ruptured blood vessels leak blood that clots. This causes swelling and pain.
TREATMENT
Once the details of your dog’s ear infection are known, treatment will likely consist of multiple elements that may include topical, oral, or surgical therapies.
TopicalDepending on the type and severity of ear infection, an ear cleaner may be recommended that could be medicated or non-medicated.
Typically, cleaning a dog's ears with an ear cleaner will be recommended every day or every other day while treating an ear infection. It's important to follow your veterinarian’s instructions for ear cleaner.
Ear cleaner should be done before applying medications—you don’t want to clean out the medications.
Ear medications will likely come in the form of ear drops that will come with an applicator for ease of getting the medication into your pup's ear canal. Depending on the type of ear infection, ear medications may be an antibiotic, anti-fungal, or both.
Some medications also include topical steroids to help with the itch. Ear medications are typically recommended once or twice a day for seven to 10 days, so it’s important to follow your veterinarian’s specific instructions.
Oral
Depending on the severity of your dog's ear infection, an oral antibiotic, antifungal, or a steroid medication may be used.
Surgical
Ears that have had severe chronic disease may no longer respond to medical treatments.
The goal of surgery for these ears is to open a pup's ear canal or sometimes to completely remove all diseased tissue. This procedure is called a total ear canal ablation (TECA) and ventral bulla osteotomy (VBO).
Recover and Management
Most dogs recover uneventfully from ear infections. However, if your dog is having frequent or chronic ear infections, your vet will likely recommend additional testing to determine if there is an underlying cause. Long-term management may include weekly preventative cleaning of the ears and/or diet change.
For our 2 older pugs who have regular ear infections (due to allergies), we have our vet administer regular Cytopoint shots
Prevention
Regular grooming, ear cleaning and ear maintenance are important parts of pet care. This is especially important if your dog swims frequently. Cleaning is best accomplished with a vet-approved ear cleaning product made specifically for pups. These typically have been specifically formulated for effective pH ranges for dogs and contain drying agents. We use this ear cleaner unless a pug is recovering from an infection, in which case we use the ear cleaner recommended by vet. The isues we have dealt with over the years involve mites and allergies. Some of the infections became quite bad where the entire ear canal became swollen shut -- in this instance, we wish we had visited the vet sooner. It's important to check the ears regularly. Remember, what you see on the surface is nothing. Reexamine photos and videos of the pug's ear canal to understand more.
Often, an underlying problem leads to the inability of the normal protective barrier of a dog’s ear to work properly. Once the ear becomes moist or inflamed, it's easy for bacteria or yeast to overgrow and cause infection in a pup.
- Foreign bodies (grass awn, foxtails) that get into the ear
- Ear mites
- Excessive moisture from bathing or swimming
- Food allergies
- Environmental allergies
- Endocrine issues such as hypothyroidism
- Autoimmune diseases such as pemphigus, lupus, or vasculitis
- Polyps (fleshy growths inside the ear canal)
- Certain types of cancer
- Trauma to the ear
These issues can make the ear canal vulnerable to a bacterial infection and/or a yeast infection.
When a dog is in pain and scratching and shaking excessively, an aural hematoma can develop. This is seen in the pinna or earflap, where ruptured blood vessels leak blood that clots. This causes swelling and pain.
TREATMENT
Once the details of your dog’s ear infection are known, treatment will likely consist of multiple elements that may include topical, oral, or surgical therapies.
TopicalDepending on the type and severity of ear infection, an ear cleaner may be recommended that could be medicated or non-medicated.
Typically, cleaning a dog's ears with an ear cleaner will be recommended every day or every other day while treating an ear infection. It's important to follow your veterinarian’s instructions for ear cleaner.
Ear cleaner should be done before applying medications—you don’t want to clean out the medications.
Ear medications will likely come in the form of ear drops that will come with an applicator for ease of getting the medication into your pup's ear canal. Depending on the type of ear infection, ear medications may be an antibiotic, anti-fungal, or both.
Some medications also include topical steroids to help with the itch. Ear medications are typically recommended once or twice a day for seven to 10 days, so it’s important to follow your veterinarian’s specific instructions.
Oral
Depending on the severity of your dog's ear infection, an oral antibiotic, antifungal, or a steroid medication may be used.
Surgical
Ears that have had severe chronic disease may no longer respond to medical treatments.
The goal of surgery for these ears is to open a pup's ear canal or sometimes to completely remove all diseased tissue. This procedure is called a total ear canal ablation (TECA) and ventral bulla osteotomy (VBO).
Recover and Management
Most dogs recover uneventfully from ear infections. However, if your dog is having frequent or chronic ear infections, your vet will likely recommend additional testing to determine if there is an underlying cause. Long-term management may include weekly preventative cleaning of the ears and/or diet change.
For our 2 older pugs who have regular ear infections (due to allergies), we have our vet administer regular Cytopoint shots
Prevention
Regular grooming, ear cleaning and ear maintenance are important parts of pet care. This is especially important if your dog swims frequently. Cleaning is best accomplished with a vet-approved ear cleaning product made specifically for pups. These typically have been specifically formulated for effective pH ranges for dogs and contain drying agents. We use this ear cleaner unless a pug is recovering from an infection, in which case we use the ear cleaner recommended by vet. The isues we have dealt with over the years involve mites and allergies. Some of the infections became quite bad where the entire ear canal became swollen shut -- in this instance, we wish we had visited the vet sooner. It's important to check the ears regularly. Remember, what you see on the surface is nothing. Reexamine photos and videos of the pug's ear canal to understand more.
Eye Injuries
A problem that is unique to Pugs is the risk of eye injury. The shape of the Pug’s skull makes their eye sockets very shallow, which means their eyelids are often not big enough to completely close. As a result, it’s easy for their eyes to get scratched, punctured, or even pop out.
There is a wonderful reference book, The Blue Book: Ocular Disorders Assumed to be Inherited in Purebred Dogs. You can download the PDF if you are interested in learning more beyond what we have posted on this page.
A problem that is unique to Pugs is the risk of eye injury. The shape of the Pug’s skull makes their eye sockets very shallow, which means their eyelids are often not big enough to completely close. As a result, it’s easy for their eyes to get scratched, punctured, or even pop out.
There is a wonderful reference book, The Blue Book: Ocular Disorders Assumed to be Inherited in Purebred Dogs. You can download the PDF if you are interested in learning more beyond what we have posted on this page.
All of a pug's eye injuries (whether a scratch, puncture or any squinting, or even the eye popping out) constitute an emergency, and your pet should be taken to the vet immediately. Without rapid treatment, these injuries can result in permanent damage or even loss of an eye.
As soon as we see squinting, we take this seriously. We never ignore squinting. That's why we keep Teramycin on hand-- even when we travel -- and we schedule a visit to the vet right away to know if we're dealing with an ulcer or other condition. Until we get to the vet, we administer Terramycin eye ointment. The type of eye ointment you use is important (avoiding steroids for some injuries) so it is imperative that you have your vet do a stain and examine the eye to know the best treatment.
As soon as we see squinting, we take this seriously. We never ignore squinting. That's why we keep Teramycin on hand-- even when we travel -- and we schedule a visit to the vet right away to know if we're dealing with an ulcer or other condition. Until we get to the vet, we administer Terramycin eye ointment. The type of eye ointment you use is important (avoiding steroids for some injuries) so it is imperative that you have your vet do a stain and examine the eye to know the best treatment.
Entropion
Read more about this condition on The Pug Dog Club of America's website.
Entropion is when a dog’s eyelid grows inward so their eyelashes rub against their cornea (clear part of the eye covering the iris). It is the most common eyelid abnormality in dogs. Entropion may affect any part of the lower eyelid, upper eyelid, or both.
Entropion in dogs can develop as a primary disease that’s genetically inherited at birth or as a secondary disease affecting dogs at any point of their lives.
SYMPTOMS
The main symptom of entropion is an inverted eyelid (turned inward) that causes eye irritation. Additional symptoms include:
CAUSES
Entropion is caused by an eyelid that has an abnormal shape in relation to the eyeball. The factors that lead to entropion in dogs include:
Primary entropion is the most common lid disease in purebred dogs affecting many breeds including the pug. It is thought to be due to a hereditary defect, but the genetic basis is not well understood. Support the Pug Dog Club of America's efforts in health research! Click here to donate.
Secondary causes of entropion in dogs include:
TREATMENT
Entropion requires surgery to be treated. The surgery involves removing the extra skin surrounding the eyelids to tighten them back to a normal anatomical position. In growing puppies under 12 weeks of age, eyelid-tacking procedures are typically performed instead of the normal surgery to treat entropion. With eyelid tacking, the skin surrounding the eye is not removed the way it is with a normal entropion surgical procedure. Instead, the excess skin surrounding the eye is temporarily turned outward with tension sutures. This is so a puppy’s facial features can fully develop without the risk of malformations due to surgical removal of the developing eyelid muscle or tissue.
Surgical complications from entropion surgery include:
Recovery from entropion surgery is rapid. Your dog’s eyes will be swollen from surgery and will be the most swollen around 24 hours after surgery. The swelling can take 2-4 weeks to completely go away. Your dog will need to wear an Elizabethan collar after surgery to protect the sutures around their eyes.
Your vet might prescribe topical eye medications depending on whether your dog has underlying corneal disease. They might also prescribe oral antibiotics, anti-inflammatories, and analgesics.
You will need to go back to the vet so they can remove the sutures 14 days after surgery, and the Elizabethan collar can be removed a few days after that.
One thing you need to watch out for is keeping your dog from injuring the incision site, which usually happens if your dog is able to remove the Elizabethan collar or if you’ve taken it off your dog too soon after the surgical procedure.Can a dog outgrow entropion?No, dogs cannot outgrow entropion. If the condition is left without corrective surgery, it can cause further eye diseases, such as corneal ulcers, conjunctivitis, and chronic eye discharge. The entropion itself can even worsen over time in breeds that develop more skin folds around their face as they age.
Is entropion in dogs painful?Yes, entropion is painful to dogs. It causes discomfort due to the constant irritation of the cornea resulting in eye damage and vision loss.
Cost? Typical surgery for entropion costs $500-$1000 per eye. A general veterinary practitioner that is familiar with entropion surgery will be able to perform the procedure for less money than a board-certified veterinary ophthalmologist.
Read more about this condition on The Pug Dog Club of America's website.
Entropion is when a dog’s eyelid grows inward so their eyelashes rub against their cornea (clear part of the eye covering the iris). It is the most common eyelid abnormality in dogs. Entropion may affect any part of the lower eyelid, upper eyelid, or both.
Entropion in dogs can develop as a primary disease that’s genetically inherited at birth or as a secondary disease affecting dogs at any point of their lives.
SYMPTOMS
The main symptom of entropion is an inverted eyelid (turned inward) that causes eye irritation. Additional symptoms include:
- Excessive tear production and staining
- Eye discharge (pus/mucus)
- Eye redness (conjunctival hyperemia)
- Keeping the eye closed
CAUSES
Entropion is caused by an eyelid that has an abnormal shape in relation to the eyeball. The factors that lead to entropion in dogs include:
- Length of eyelid
- Shape of skull
- Shape of the bone cavity that contains the eyeball
- Gender
- Extensive skin folds and wrinkles around the eyes
- Entropion in dogs can be primary, or present at birth, or secondary, meaning it was caused by something else.
Primary entropion is the most common lid disease in purebred dogs affecting many breeds including the pug. It is thought to be due to a hereditary defect, but the genetic basis is not well understood. Support the Pug Dog Club of America's efforts in health research! Click here to donate.
Secondary causes of entropion in dogs include:
- Trauma or inflammation from eye injuries
- Eyelid scarring or nerve damage
- Infectious disease
- Systemic dermatological conditions, such as generalized pyoderma, demodectic mange, or dermatophytosis (ringworm)
TREATMENT
Entropion requires surgery to be treated. The surgery involves removing the extra skin surrounding the eyelids to tighten them back to a normal anatomical position. In growing puppies under 12 weeks of age, eyelid-tacking procedures are typically performed instead of the normal surgery to treat entropion. With eyelid tacking, the skin surrounding the eye is not removed the way it is with a normal entropion surgical procedure. Instead, the excess skin surrounding the eye is temporarily turned outward with tension sutures. This is so a puppy’s facial features can fully develop without the risk of malformations due to surgical removal of the developing eyelid muscle or tissue.
Surgical complications from entropion surgery include:
- Under correction, which occurs if not enough eyelid skin has been removed to correct the eyelid from rubbing the cornea
- Overcorrection, which occurs if too much eyelid skin is removed, preventing the eyelids from closing normally
Recovery from entropion surgery is rapid. Your dog’s eyes will be swollen from surgery and will be the most swollen around 24 hours after surgery. The swelling can take 2-4 weeks to completely go away. Your dog will need to wear an Elizabethan collar after surgery to protect the sutures around their eyes.
Your vet might prescribe topical eye medications depending on whether your dog has underlying corneal disease. They might also prescribe oral antibiotics, anti-inflammatories, and analgesics.
You will need to go back to the vet so they can remove the sutures 14 days after surgery, and the Elizabethan collar can be removed a few days after that.
One thing you need to watch out for is keeping your dog from injuring the incision site, which usually happens if your dog is able to remove the Elizabethan collar or if you’ve taken it off your dog too soon after the surgical procedure.Can a dog outgrow entropion?No, dogs cannot outgrow entropion. If the condition is left without corrective surgery, it can cause further eye diseases, such as corneal ulcers, conjunctivitis, and chronic eye discharge. The entropion itself can even worsen over time in breeds that develop more skin folds around their face as they age.
Is entropion in dogs painful?Yes, entropion is painful to dogs. It causes discomfort due to the constant irritation of the cornea resulting in eye damage and vision loss.
Cost? Typical surgery for entropion costs $500-$1000 per eye. A general veterinary practitioner that is familiar with entropion surgery will be able to perform the procedure for less money than a board-certified veterinary ophthalmologist.
Corneal Ulcers
If you see your Pug squinting or the eye seems red or weepy, he may have a scratch or ulcer on his cornea (the clear part of the eye). Your vet may want to put special stain on the eye to observe the ulcer and will send home medication. Ulcers can deepen quickly and the eye can rupture so you should seek veterinary care right away. Learn more on The Pug Dog Club of America's website.
If you see your Pug squinting or the eye seems red or weepy, he may have a scratch or ulcer on his cornea (the clear part of the eye). Your vet may want to put special stain on the eye to observe the ulcer and will send home medication. Ulcers can deepen quickly and the eye can rupture so you should seek veterinary care right away. Learn more on The Pug Dog Club of America's website.
Dystichia
You can learn more about this eye condition on The Pug Dog Club of America's website. Sometimes Pugs have extra eye lashes that rub against the eye and can cause irritation, and sometimes ulcers. Some dogs require surgery to remove the offending lashes.
You can learn more about this eye condition on The Pug Dog Club of America's website. Sometimes Pugs have extra eye lashes that rub against the eye and can cause irritation, and sometimes ulcers. Some dogs require surgery to remove the offending lashes.
Proptosis
Because Pug eyes tend to protrude, it is easier to have them forced from the eye socket than with other breeds. If a Pug is bitten near the eye, the eye could be pushed forward in front of the lids. The eye is still held in place by nerves and muscles, but it is often too damaged to be sighted. This is a medical emergency since rapid response may allow surgical replacement and some sight might be saved. Learn more on The Pug Dog Club of America's website.
Because Pug eyes tend to protrude, it is easier to have them forced from the eye socket than with other breeds. If a Pug is bitten near the eye, the eye could be pushed forward in front of the lids. The eye is still held in place by nerves and muscles, but it is often too damaged to be sighted. This is a medical emergency since rapid response may allow surgical replacement and some sight might be saved. Learn more on The Pug Dog Club of America's website.
DRY EYE (KERATOCONJUNCTIVITIS SICCA OR KCS) AND PIGMENTARY KERATOPATHY (PK)
Commonly seen in Pugs, these two problems often, but not always, occur together. Some Pugs don’t produce enough tears to keep their eyes moist and have KCS. You may see excessive mucous in your Pugs eyes and they may be red. Your vet can do a special test called a Schirmer Tear Test to determine if your Pug is affected. If he isn’t producing enough tears, there are medications available that will stimulate the tear glands to produce more. You usually need to keep the excess mucous flushed out of the eyes as well. With PK, owners sometimes see dark black spots on the cornea or clear part of the eye, especially in the corner near the nose. Sometimes there is just a little bit near the inside corner, but some Pugs have the pigment cover their corneas and they are blind. Medications can help keep the eyes moist and disperse the pigment. Both of these problems require life-long therapy.Dry Eye and Pigmentary Keratopathy. (Cyclosporine is approved to treat dry eye (keratoconjunctivitis sicca) and CSK (chronic superficial keratitis) in dogs. It is also useful in treating immune-mediated keratitis and pannus in horses and dogs. You and your veterinarian will discuss why this drug is the most appropriate choice. (NOTE: Sometimes your vet can send rx to certain human pharmacies who can fill this a bit cheaper. Ask your vet if this is an option in your area.)
Commonly seen in Pugs, these two problems often, but not always, occur together. Some Pugs don’t produce enough tears to keep their eyes moist and have KCS. You may see excessive mucous in your Pugs eyes and they may be red. Your vet can do a special test called a Schirmer Tear Test to determine if your Pug is affected. If he isn’t producing enough tears, there are medications available that will stimulate the tear glands to produce more. You usually need to keep the excess mucous flushed out of the eyes as well. With PK, owners sometimes see dark black spots on the cornea or clear part of the eye, especially in the corner near the nose. Sometimes there is just a little bit near the inside corner, but some Pugs have the pigment cover their corneas and they are blind. Medications can help keep the eyes moist and disperse the pigment. Both of these problems require life-long therapy.Dry Eye and Pigmentary Keratopathy. (Cyclosporine is approved to treat dry eye (keratoconjunctivitis sicca) and CSK (chronic superficial keratitis) in dogs. It is also useful in treating immune-mediated keratitis and pannus in horses and dogs. You and your veterinarian will discuss why this drug is the most appropriate choice. (NOTE: Sometimes your vet can send rx to certain human pharmacies who can fill this a bit cheaper. Ask your vet if this is an option in your area.)
Brachycephalic Airway Syndrome (BOAS)
To learn even more, you can visit The Pug Dog Club of America's website.
Brachycephalic is a term that refers to dog breeds with shortened snouts and flat faces. The term brachycephalic comes from the Greek words brachy, meaning short, and cephalic, meaning head.
Brachycephalic airway syndrome refers to a specific combination of abnormalities affecting a dog’s airway and breathing, resulting from selectively breeding for this appearance. Their unique smooshed face is a result of shortened skull, facial, and nasal bones. This structural shortening of the face also results in anatomical changes to their throat and airways, creating brachycephalic airway syndrome.
Specifically, the condition refers to the combination of three functional abnormalities:
How Veterinarians Diagnose Brachycephalic Airway SyndromeDiagnosis will be largely based on the dog’s breed, clinical signs, and physical examination findings, such as stenotic nares (narrowed nostrils). A classic breathing noise characterized as a low-pitched, snoring-type sound called stertor may be noted in dogs with brachycephalic airway syndrome.
Your veterinarian may want to perform a sedated oral examination to evaluate for elongated soft palate and everted laryngeal saccules. An x-ray of the neck and chest may also visualize the trachea (windpipe) and assess the heart and lungs. A complete blood count, serum blood chemistry, and urinalysis will likely be recommended for a baseline evaluation.
Treatment of Brachycephalic Airway SyndromeMedical management may be an option if clinical signs are mild or infrequent. Excessive weight worsens the symptoms, so medical management for brachycephalic airway syndrome includes weight loss if your dog is overweight or obese. Heat and humidity can also worsen clinical signs, so care should be taken to limit time outside during hot summer days. Excessive exercise can increase stress of breathing and may exacerbate brachycephalic airway syndrome.
If your dog is having trouble breathing while at the vet, they may utilize mild sedatives to help your dog calm down and breathe easier. Additional therapy may be initiated if appropriate, including steroids, oxygen, and cooling measures, all designed to alleviate acute respiratory distress. Medication may also be administered to address any gastrointestinal signs, such as vomiting.
Surgery may be considered if the structural abnormalities cause distress to your dog, become worse over time, or result in life-threatening trouble breathing from upper airway blockage. Life-threatening would be defined as more than one episode where your pet has had trouble breathing and needed medical assistance. Multiple procedures are usually required to alleviate the signs of brachycephalic airway syndrome, and include:
How Much Does Brachycephalic Airway Syndrome Surgery Cost?The cost of surgery for brachycephalic airway syndrome can vary depending on many factors, including geographic location, how sick the dog is, and how extensive the procedure needs to be. However, if all three procedures are performed, pet parents can likely expect to paya total between $3,000 and $5,000.
Pet insurance may be a good idea to help offset anticipated costs and illnesses related to getting a new pup. However, when it comes to inherited and breed-related conditions (like brachycephalic airway syndrome), not all policies offer coverage if conditions are considered pre-existing. Make sure that any pet insurance policy you consider covers brachycephalic dogs and brachycephalic airway syndrome.
Recovery and Management of Brachycephalic Airway SyndromeDogs undergoing brachycephalic airway surgery are monitored carefully after surgery, as inflammation and bleeding are possible. Typically, they will remain hospitalized in a 24-hour ICU for 1-2 days of observation.
The prognosis is good for young dogs, and most pet parents see a significant improvement in their breathing and ability to exercise. However, prognosis may be more guarded in older dogs with a chronic history of trouble breathing, especially if they have started to develop laryngeal collapse. In cases of advanced laryngeal collapse, a tube may need to be inserted in the neck (permanent tracheostomy) to provide improvement in breathing.
For long-term management, it’s crucial to keep brachycephalic dogs lean and at an appropriate weight. Working with your vet on a weight goal and, if needed, a weight loss plan may be very beneficial. A harness collar is recommended to take pressure off the neck as seen with a traditional neck collar.
Extreme care should always be taken to ensure that brachycephalic dogs do not overheat. Minimal activity or time outside during hot and humid weather is recommended, and always have plenty of fresh water and access to shade.
To learn even more, you can visit The Pug Dog Club of America's website.
Brachycephalic is a term that refers to dog breeds with shortened snouts and flat faces. The term brachycephalic comes from the Greek words brachy, meaning short, and cephalic, meaning head.
Brachycephalic airway syndrome refers to a specific combination of abnormalities affecting a dog’s airway and breathing, resulting from selectively breeding for this appearance. Their unique smooshed face is a result of shortened skull, facial, and nasal bones. This structural shortening of the face also results in anatomical changes to their throat and airways, creating brachycephalic airway syndrome.
Specifically, the condition refers to the combination of three functional abnormalities:
- Stenotic nares: Referring to narrow nostrils or small nostril openings. This results in a decreased ability to breathe through the nose and restricted airflow, which leads to increased panting and a higher risk of overheating.
- Elongated soft palate: The soft palate is the part of the roof of the mouth made up of tissue that separates the nasal passage from the oral cavity. Given brachycephalic dogs’ shorter snout, the soft palate is often too long for the length of their mouth. The excess flaps into the throat, causing snoring sounds and blocking airflow into the windpipe and lungs.
- Everted laryngeal saccules: In normal anatomy, there are two small pockets (saccules) in the back of the throat. In brachycephalic dogs, there is an increased effort to breathe due to the stenotic nares and elongated soft palate. This increased effort to breathe can cause the saccules to turn inside out and further block the airway.
- Hypoplastic trachea: This means the trachea, or windpipe, is congenitally smaller in diameter than normal. This can make it harder for dogs to breathe in enough air with each breath (like breathing through a straw).
- Laryngeal collapse: The larynx, or voice box, can become damaged by chronic stress to the cartilage from working too hard to breathe. Laryngeal collapse leads to more blockage of the airway, and potentially trouble breathing.
- Affenpinscher
- Boston Terrier
- Boxer
- Bullmastiff
- Brussels Griffon
- Cane Corso
- Chow Chow
- Dogue de Bordeaux
- English Bulldog
- English Toy Spaniel
- French Bulldog
- Japanese Chin
- Lhasa Apso
- Pekingese
- Pug
- Shih Tzu
- Noisy breathing
- Snoring
- Gagging or retching
- Coughing
- Trouble breathing or increased effort to breathe
- Increased panting
- Exercise intolerance (tire easily with exercise)
- Distended abdomen or vomiting from swallowing too much air while working to breathe
- Overheating
- Pale or blue gums
- Collapse
How Veterinarians Diagnose Brachycephalic Airway SyndromeDiagnosis will be largely based on the dog’s breed, clinical signs, and physical examination findings, such as stenotic nares (narrowed nostrils). A classic breathing noise characterized as a low-pitched, snoring-type sound called stertor may be noted in dogs with brachycephalic airway syndrome.
Your veterinarian may want to perform a sedated oral examination to evaluate for elongated soft palate and everted laryngeal saccules. An x-ray of the neck and chest may also visualize the trachea (windpipe) and assess the heart and lungs. A complete blood count, serum blood chemistry, and urinalysis will likely be recommended for a baseline evaluation.
Treatment of Brachycephalic Airway SyndromeMedical management may be an option if clinical signs are mild or infrequent. Excessive weight worsens the symptoms, so medical management for brachycephalic airway syndrome includes weight loss if your dog is overweight or obese. Heat and humidity can also worsen clinical signs, so care should be taken to limit time outside during hot summer days. Excessive exercise can increase stress of breathing and may exacerbate brachycephalic airway syndrome.
If your dog is having trouble breathing while at the vet, they may utilize mild sedatives to help your dog calm down and breathe easier. Additional therapy may be initiated if appropriate, including steroids, oxygen, and cooling measures, all designed to alleviate acute respiratory distress. Medication may also be administered to address any gastrointestinal signs, such as vomiting.
Surgery may be considered if the structural abnormalities cause distress to your dog, become worse over time, or result in life-threatening trouble breathing from upper airway blockage. Life-threatening would be defined as more than one episode where your pet has had trouble breathing and needed medical assistance. Multiple procedures are usually required to alleviate the signs of brachycephalic airway syndrome, and include:
- Stenotic nares resection: Surgically widening the nostrils.
- Soft palate resection (staphylectomy): Surgical trimming of the soft palate to shorten the tissue.
- Laryngeal saccule removal: Removing the everted saccules.
How Much Does Brachycephalic Airway Syndrome Surgery Cost?The cost of surgery for brachycephalic airway syndrome can vary depending on many factors, including geographic location, how sick the dog is, and how extensive the procedure needs to be. However, if all three procedures are performed, pet parents can likely expect to paya total between $3,000 and $5,000.
Pet insurance may be a good idea to help offset anticipated costs and illnesses related to getting a new pup. However, when it comes to inherited and breed-related conditions (like brachycephalic airway syndrome), not all policies offer coverage if conditions are considered pre-existing. Make sure that any pet insurance policy you consider covers brachycephalic dogs and brachycephalic airway syndrome.
Recovery and Management of Brachycephalic Airway SyndromeDogs undergoing brachycephalic airway surgery are monitored carefully after surgery, as inflammation and bleeding are possible. Typically, they will remain hospitalized in a 24-hour ICU for 1-2 days of observation.
The prognosis is good for young dogs, and most pet parents see a significant improvement in their breathing and ability to exercise. However, prognosis may be more guarded in older dogs with a chronic history of trouble breathing, especially if they have started to develop laryngeal collapse. In cases of advanced laryngeal collapse, a tube may need to be inserted in the neck (permanent tracheostomy) to provide improvement in breathing.
For long-term management, it’s crucial to keep brachycephalic dogs lean and at an appropriate weight. Working with your vet on a weight goal and, if needed, a weight loss plan may be very beneficial. A harness collar is recommended to take pressure off the neck as seen with a traditional neck collar.
Extreme care should always be taken to ensure that brachycephalic dogs do not overheat. Minimal activity or time outside during hot and humid weather is recommended, and always have plenty of fresh water and access to shade.
Pug Orthopedics
While Pugs tend to be sturdy little dogs, they can face some serious problems with their bones and legs.
Hemivertebrae
This is a condition involving deformed, misshaped vertebrae or bones of the spine. It is commonly seen in all of the short-faced breeds like Pugs, Bulldogs and French Bulldogs. Some animals will have a few odd vertebrae and be completely normal. Others will start having problems between 4 and 6 months of age. The puppy may have a staggering, uncoordinated, weak gait. Some puppies get progressively worse and some actually become paralyzed. There is a study being conducted in England on this condition but right now we don’t know much about why some dogs have trouble with this and others don’t. Some specialists recommend spine surgery to stabilize the affected area but each case must be carefully evaluated.
While Pugs tend to be sturdy little dogs, they can face some serious problems with their bones and legs.
Hemivertebrae
This is a condition involving deformed, misshaped vertebrae or bones of the spine. It is commonly seen in all of the short-faced breeds like Pugs, Bulldogs and French Bulldogs. Some animals will have a few odd vertebrae and be completely normal. Others will start having problems between 4 and 6 months of age. The puppy may have a staggering, uncoordinated, weak gait. Some puppies get progressively worse and some actually become paralyzed. There is a study being conducted in England on this condition but right now we don’t know much about why some dogs have trouble with this and others don’t. Some specialists recommend spine surgery to stabilize the affected area but each case must be carefully evaluated.
Hip Dysplasia
Pugs are second only to Bulldogs with the amount of hip dysplasia in the breed (approximately 62%). There are many factors, including genetics, environment and nutrition that contribute to this deformity of the hip joint. Research on larger breeds has shown that switching to adult food early in a puppy’s life (12 to 16 weeks), avoiding supplements and keeping the puppy thin as it is growing will minimize its chance of being affected. Even though many Pugs are affected, most are able to lead normal, healthy lives even with the problem, unlike some of the large and giant breeds, who require surgery to get around easily. More and more breeders are including hip xray screening in the health testing for pugs in their breeding program. We include this at Pickwick Pugs and our standards are high.
Pugs are second only to Bulldogs with the amount of hip dysplasia in the breed (approximately 62%). There are many factors, including genetics, environment and nutrition that contribute to this deformity of the hip joint. Research on larger breeds has shown that switching to adult food early in a puppy’s life (12 to 16 weeks), avoiding supplements and keeping the puppy thin as it is growing will minimize its chance of being affected. Even though many Pugs are affected, most are able to lead normal, healthy lives even with the problem, unlike some of the large and giant breeds, who require surgery to get around easily. More and more breeders are including hip xray screening in the health testing for pugs in their breeding program. We include this at Pickwick Pugs and our standards are high.
Legg-Perthes
This is another disease involving the hip joint and is seen in many of the toy breeds. In this disease, the blood supply to the head of the femur (the large rear leg bone) gets compromised and the head of the femur that connects to the pelvis starts to disintegrate. This usually is first noticeable in puppies 4 to 6 months of age as they start limping and getting muscle atrophy of the leg. The surgery to help the puppy involves cutting the diseased head off of the femur so it is no longer attached to the pelvis. Scar tissue comes in and forms a “false joint” and the puppy is usually pain free. At Pickwick Pugs we had to deal with this with a young pug we purchased from another breeder in Mississippi. The cost of the surgery was tremendous and the rehabilitation even more expensive, however, the pug can walk and run thanks to our efforts. We were told by 4 vets (including 2 of the most widely known orthapedic surgeons in the Southeast) that it was 'textbook case genetic' with the pug we purchased, but this can also be a result of the pug falling or injuring itself. This is one reason it is so important to add ramps to sofas and not allow your pug puppy to jump off of high furniture and such. Protect your pug's joints -- and you'll protect your wallet! Also, only buy from breeders who include xrays of patella/hips/spine and other health screening. The breeder we purchased our pug with Legg-Calves-Perthes did not believe in health testing.
This is another disease involving the hip joint and is seen in many of the toy breeds. In this disease, the blood supply to the head of the femur (the large rear leg bone) gets compromised and the head of the femur that connects to the pelvis starts to disintegrate. This usually is first noticeable in puppies 4 to 6 months of age as they start limping and getting muscle atrophy of the leg. The surgery to help the puppy involves cutting the diseased head off of the femur so it is no longer attached to the pelvis. Scar tissue comes in and forms a “false joint” and the puppy is usually pain free. At Pickwick Pugs we had to deal with this with a young pug we purchased from another breeder in Mississippi. The cost of the surgery was tremendous and the rehabilitation even more expensive, however, the pug can walk and run thanks to our efforts. We were told by 4 vets (including 2 of the most widely known orthapedic surgeons in the Southeast) that it was 'textbook case genetic' with the pug we purchased, but this can also be a result of the pug falling or injuring itself. This is one reason it is so important to add ramps to sofas and not allow your pug puppy to jump off of high furniture and such. Protect your pug's joints -- and you'll protect your wallet! Also, only buy from breeders who include xrays of patella/hips/spine and other health screening. The breeder we purchased our pug with Legg-Calves-Perthes did not believe in health testing.
Legg-Calve-Perthes Disease (LCP) is a disorder of hip joint conformation occurring in both humans and dogs. In dogs, it is most often seen in the miniature and toy breeds between the ages of 4 months to a year.
LCP results when the blood supply to the femoral head is interrupted resulting in avascular necrosis, or the death of the bone cells. Followed by a period of revascularization, the femoral head is subject to remodeling and/or collapse creating an irregular fit in the acetabulum, or socket. This process of bone cells dying and fracturing followed by new bone growth and remodeling of the femoral head and neck, can lead to stiffness and pain.
LCP is believed to be an inherited disease, although the mode of inheritance is not known. Because there is a genetic component, it is recommended that dogs affected with LCP not be used in breeding programs.
We dealt with this disease when we purchased a show prospect male pug puppy from a breeder in Mississippi. We trained him and he was doing well but then we noticed that he was starting to side wind or 'crab' walk, seeming to favor leg or hip. We consulted 6 different vets, 3 of whom were ortho specialists. The final vet, who is considered the best orthopedic surgeon in the Southeast, verified what other vets had said ... that it was a "textbook case genetic case". After x-rays with each vet, over a period of 2 days, the final vet said that the bone was so diseased that it was a miracle the leg had not snapped and that it was just holding on by a thread. He explained that we needed to do the surgery immediately, which involved the excision of the femoral head and neck. By removing the femoral head and neck, the bone on bone contact that is the source of the pain and discomfort is eliminated. Later, through the healing process and with therapy, a new false joint is formed by muscle and tissue, and the dog may have a complete recovery. Indeed, Randolph can now walk, run, and live a normal life thanks to this surgery and subsequent physical therapy. If he had been a larger dog, a total hip replacement would have been required which would have involved traveling to another state, staying in a hotel, and ofcourse an even more expensive surgery. We paid over $6,000 all said and done (in addition to the $3,000 to buy the puppy).
Another long time breeder in a different state told us that they had never dealt with LCP in a specific line of pugs for generations and generations. Suddenly it appeared with a puppy -- out of no where. So, it is a concern in the breed (and other breeds) and can rear its head unexpectedly.
This is one reason we include OFA hip, patellar, spine, X-rays with the health screening of all the pugs in our breeding program. We use Blue Ridge Veterinary Imaging and the same radiographic image can be used to evaluate the presence of both LCP and hip dysplasia.
Here is more about continued study on LCP.
LCP results when the blood supply to the femoral head is interrupted resulting in avascular necrosis, or the death of the bone cells. Followed by a period of revascularization, the femoral head is subject to remodeling and/or collapse creating an irregular fit in the acetabulum, or socket. This process of bone cells dying and fracturing followed by new bone growth and remodeling of the femoral head and neck, can lead to stiffness and pain.
LCP is believed to be an inherited disease, although the mode of inheritance is not known. Because there is a genetic component, it is recommended that dogs affected with LCP not be used in breeding programs.
We dealt with this disease when we purchased a show prospect male pug puppy from a breeder in Mississippi. We trained him and he was doing well but then we noticed that he was starting to side wind or 'crab' walk, seeming to favor leg or hip. We consulted 6 different vets, 3 of whom were ortho specialists. The final vet, who is considered the best orthopedic surgeon in the Southeast, verified what other vets had said ... that it was a "textbook case genetic case". After x-rays with each vet, over a period of 2 days, the final vet said that the bone was so diseased that it was a miracle the leg had not snapped and that it was just holding on by a thread. He explained that we needed to do the surgery immediately, which involved the excision of the femoral head and neck. By removing the femoral head and neck, the bone on bone contact that is the source of the pain and discomfort is eliminated. Later, through the healing process and with therapy, a new false joint is formed by muscle and tissue, and the dog may have a complete recovery. Indeed, Randolph can now walk, run, and live a normal life thanks to this surgery and subsequent physical therapy. If he had been a larger dog, a total hip replacement would have been required which would have involved traveling to another state, staying in a hotel, and ofcourse an even more expensive surgery. We paid over $6,000 all said and done (in addition to the $3,000 to buy the puppy).
Another long time breeder in a different state told us that they had never dealt with LCP in a specific line of pugs for generations and generations. Suddenly it appeared with a puppy -- out of no where. So, it is a concern in the breed (and other breeds) and can rear its head unexpectedly.
This is one reason we include OFA hip, patellar, spine, X-rays with the health screening of all the pugs in our breeding program. We use Blue Ridge Veterinary Imaging and the same radiographic image can be used to evaluate the presence of both LCP and hip dysplasia.
Here is more about continued study on LCP.
It was difficult to watch (FYI we NEVER recommend jerking a lead like this with any dog but especially with a pug.) When we returned home we immediately sought out a vet, then another vet, and then 2 more vets as we were bumped up to specialists. It was serious and we are so glad we did not listen to the breeder who maintained there was nothing wrong with him, just that we didn't jerk the lead correctly. The final ortho specialist on the 2nd day after returning home said that we needed to do the surgery right away (that day) because it was miraculous the bone had not snapped. It was completely diseased. We contacted the breeder after each vet visit with updates. We have spoken with many longtime breeders since then and they have all stated that LCP can pop up generations into a line .... parents, grandparents, great grandparents, great great grandparents can all be fine with no puppies presenting with LCP and then boom. So, we understand the breeder had no control over this as it is a recessive gene and can 'popup" unexpectedly. However, we are also thankful we listened to our gut and sought out veterinarians to help when we knew something was wrong. It's important to listen to your gut when dealing with caring for your furbabies.
Luxating Patellas
This involves the stifle or knee joint of many of the toy breeds and even some larger ones. The patella or kneecap usually rides up and down in a groove on the front of the knee. With this condition, the kneecap slides to the side (usually the inside) and the joint is unstable. When the kneecap is out, the dog may limp and carry the leg. The dog can often stretch his leg back and pop the patella back in himself. Some dogs are normal when young and develop this with age. Many dogs live their lives with this but some require surgery to deepen the groove and reposition the patella so it stays in place. One or both legs may be affected. We have had one pug (our rescue pug Charlie) who had to have this surgery done. Both were weak but we only did the surgery on the one that was really suffering and disclocating. He was fine for the rest of his life with having done just the one surgery. The recovery is tought as they are crate confined. We have had one Pickwick pug puppy who does a lot of agility who had this surgery done as well and made a complete recovery. We have never bred a pug with any indication of luxating patellar and we use Blue Ridge Veterinary Imaging as their equipment is superb and high resolution images. We include this health screening in all of the pugs in our breeding program.
This involves the stifle or knee joint of many of the toy breeds and even some larger ones. The patella or kneecap usually rides up and down in a groove on the front of the knee. With this condition, the kneecap slides to the side (usually the inside) and the joint is unstable. When the kneecap is out, the dog may limp and carry the leg. The dog can often stretch his leg back and pop the patella back in himself. Some dogs are normal when young and develop this with age. Many dogs live their lives with this but some require surgery to deepen the groove and reposition the patella so it stays in place. One or both legs may be affected. We have had one pug (our rescue pug Charlie) who had to have this surgery done. Both were weak but we only did the surgery on the one that was really suffering and disclocating. He was fine for the rest of his life with having done just the one surgery. The recovery is tought as they are crate confined. We have had one Pickwick pug puppy who does a lot of agility who had this surgery done as well and made a complete recovery. We have never bred a pug with any indication of luxating patellar and we use Blue Ridge Veterinary Imaging as their equipment is superb and high resolution images. We include this health screening in all of the pugs in our breeding program.
Pug Myelopathy is a recently recognized spinal condition believed unique in Pugs. It is called by several terms, and it is most often referred to as “Pug Myelopathy”. Pug Myelopathy is considered the most frequent cause of rear limb incoordination (ataxia) and progression of paralysis of the rear limbs over a period of one to four years. Originally referred to as “Weak Rear”, this has become a widespread problem in Pugs. The rear legs appear to be weak, but the cause is a neurological deficit that develops in the spine. Affected dogs may initially drag their feet, stagger, have trouble jumping and can be fecal and urinary incontinent. It usually affects just the rear limbs, unlike a very different disease, Degenerative Myelopathy (DM), which can have similar initial signs, but progresses tragically to complete paralysis and death. In Pug Myelopathy, we are learning there is usually a complex of spinal abnormalities that involve both the vertebral bones, and can also involve compression of the spinal cord. The compression can be caused by one (or multiple lesions) that include one or multiple sites of chronic Hansen type II intervertebral disc disease (IVDD); spinal arachnoid diverticulum (SAD); spinal cord atrophy; and fibrosis of the arachnoid layer of the meninges. Unraveling the relationships between these conditions is one goal of the research at Michigan State University funded by the Pug Dog Club of America.
Other names that refer to Pug myelopathy include “Pug constrictive myelopathy (CM)”, “facet hypoplasia”, “subarachnoid diverticulum (SAD)” and others. Although little is published about this condition, Pug Myelopathy may be the most common cause of mid-back spinal cord problems in Pugs.
Another good description of the disease is provided by Southeast Veterinary Neurology, Wong M, (2017). Case History of Surgical Treatment for Pug Myelopathy. [video] Available at: www.sevneurology.com/patients/wellington/ [Accessed 10 Jul. 2017].
Many veterinarians are not yet knowledgeable about this condition, as published information is not yet widely available. Pugs with rear limb ataxia may have had a previous diagnosis that was incomplete in light of this evolving information. Since so little is known, there is no consensus among neurologists about the best way to treat it. Surgery may be appropriate for individual cases, but it must be considered as soon as possible, after symptoms first occur, and may only delay progression of paralysis.
The most important palliative treatment appears to be consistent physical therapy using rehabilitation exercises to preserve muscle strength and enhance development of a spinal walk. A wheeled cart, carefully fitted by a knowledgeable professional, may improve their ability to walk. Other forms of integrative medicine can enhance their ability and desire to stay mobile. Pugs affected with Pug Myelopathy are usually pain free and can lead excellent long lives with good nursing care. All senior Pugs require periodic wellness exams to detect and alleviate other problems of aging using medication and/or supplements. It is critical the Pug is carefully monitored for its ability to completely empty the urinary bladder several times a day. Several other well documented conditions in Pugs also cause symptoms of ataxia, including hemivertebrae (usually young dogs); acute sudden onset Intervertebral Disc Disease (IVDD) or “slipped disc” – (usually painful); spinal cord tumors; and spinal arthritis in elder dogs. It is important to have your primary care veterinarian arrange a referral for your Pug for an examination by a board certified veterinary neurologist or surgeon when symptoms of ataxia first appear.
While not diagnosed, we feel that we dealt with this back in the 1990s with our rescue pug George. You can help by contributing to the PDCA Health Research Fund. They have made great strides with health screening testing for genetic markers with PDE (Pug Dog Encephalitis) and your support will help with their efforts to learn more about this condition and hopefully develop genetic health testing and screening for breeders.
Other names that refer to Pug myelopathy include “Pug constrictive myelopathy (CM)”, “facet hypoplasia”, “subarachnoid diverticulum (SAD)” and others. Although little is published about this condition, Pug Myelopathy may be the most common cause of mid-back spinal cord problems in Pugs.
Another good description of the disease is provided by Southeast Veterinary Neurology, Wong M, (2017). Case History of Surgical Treatment for Pug Myelopathy. [video] Available at: www.sevneurology.com/patients/wellington/ [Accessed 10 Jul. 2017].
Many veterinarians are not yet knowledgeable about this condition, as published information is not yet widely available. Pugs with rear limb ataxia may have had a previous diagnosis that was incomplete in light of this evolving information. Since so little is known, there is no consensus among neurologists about the best way to treat it. Surgery may be appropriate for individual cases, but it must be considered as soon as possible, after symptoms first occur, and may only delay progression of paralysis.
The most important palliative treatment appears to be consistent physical therapy using rehabilitation exercises to preserve muscle strength and enhance development of a spinal walk. A wheeled cart, carefully fitted by a knowledgeable professional, may improve their ability to walk. Other forms of integrative medicine can enhance their ability and desire to stay mobile. Pugs affected with Pug Myelopathy are usually pain free and can lead excellent long lives with good nursing care. All senior Pugs require periodic wellness exams to detect and alleviate other problems of aging using medication and/or supplements. It is critical the Pug is carefully monitored for its ability to completely empty the urinary bladder several times a day. Several other well documented conditions in Pugs also cause symptoms of ataxia, including hemivertebrae (usually young dogs); acute sudden onset Intervertebral Disc Disease (IVDD) or “slipped disc” – (usually painful); spinal cord tumors; and spinal arthritis in elder dogs. It is important to have your primary care veterinarian arrange a referral for your Pug for an examination by a board certified veterinary neurologist or surgeon when symptoms of ataxia first appear.
While not diagnosed, we feel that we dealt with this back in the 1990s with our rescue pug George. You can help by contributing to the PDCA Health Research Fund. They have made great strides with health screening testing for genetic markers with PDE (Pug Dog Encephalitis) and your support will help with their efforts to learn more about this condition and hopefully develop genetic health testing and screening for breeders.
Pug Neurology
We're not talking about how smart and trainable Pugs are, but rather some serious problems that can occur in the central nervous system or brain of
the Pug.
We're not talking about how smart and trainable Pugs are, but rather some serious problems that can occur in the central nervous system or brain of
the Pug.
Epilepsy
Not all Pugs who have seizures have PDE. We see a number of Pugs who have idiopathic epilepsy, or seizures for no known reason. Many of these dogs can be controlled quite well on anticonvulsant medication, such as Phenobarbital or Potassium Bromide. The goal of therapy is to decrease the severity and frequency of the seizures. You will need to work closely with your vet to determine the correct drug and dosage for your pet. We have dealt with this with our pug Louis Armstrong back in the 1990s. He was a pet and neutered but at a young age (under a year) he began starting having seizures. He lived his life (13 years of age) on phenobarbital, adjusting the dosage as needed. It was hard watching him but we learned to cope. Keep them calm after a seizure and in a quiet, darker room. Let them relax and give them plenty of water. They will be quite tired after an episode.
Not all Pugs who have seizures have PDE. We see a number of Pugs who have idiopathic epilepsy, or seizures for no known reason. Many of these dogs can be controlled quite well on anticonvulsant medication, such as Phenobarbital or Potassium Bromide. The goal of therapy is to decrease the severity and frequency of the seizures. You will need to work closely with your vet to determine the correct drug and dosage for your pet. We have dealt with this with our pug Louis Armstrong back in the 1990s. He was a pet and neutered but at a young age (under a year) he began starting having seizures. He lived his life (13 years of age) on phenobarbital, adjusting the dosage as needed. It was hard watching him but we learned to cope. Keep them calm after a seizure and in a quiet, darker room. Let them relax and give them plenty of water. They will be quite tired after an episode.
Pug Dog Encephalitis (PDE)
Thankfully we have not had to deal with PDE at Pickwick Pugs but it is a problem unique to the Pug breed which we have been told is horrific to see and watch striking terror in the hearts of those of us who know and love them. PDE is a fatal inflammatory brain disease. We do not know exactly why Pugs get it. We are beginning to explore ways to treat it. There is no way to determine with accuracy if your Pug has it except with the brain tissue of dead dogs. The Pugs who are affected are usually young. The dogs will have seizures, circling, blindness, coma and death, all in the space of a few days to a few weeks. The Pug Dog Club of America, along with the American Kennel Club Canine Health Foundation, has contributed to studies which has directly led to the creation of a test for the genetic marker for PDE – or NME, Necrotizing Meningoencephalitis, as it is scientifically called. This is the first step towards identifying, understanding, treating and possibly eradicating this horrible disease from our Pug population.
At the 2023 Pug Dog Club of America National Conference, 3 of our pugs participated in an ongoing study being conducted (blog here) as healthy examines. They tested well and showed no early signs of PDE but they will continue to be tracked over the years. The more pugs involved in the study the more successful the data so contact contact Dr. Barber (see below) if you would like to participate and help.
Diagnosis:
According to UC Davis, www.vgl.ucdavis.edu/services/PDE.php , there is NO DIAGNOSTIC FOR PDE OR NME in dogs. There is only a test is only to determine ~RISK~ for developing NME in Pug Dogs and for selecting matings that will produce puppies that are at decreased risk (N/N, N/S). Although a significant proportion (11%) of Pug Dogs is S/S, only about 1 in 8 of this group will develop NME during their lifetime. Also, breeders are advised against breeding out the S genotype, because 40% of Pug Dogs have the S genotype in a heterozygous (N/S = 29%) or homozygous state (S/S = 11%). Eliminating the S genotype will lead to a considerable loss of genetic diversity. Therefore, breeders should carefully select matings that do not produce S/S puppies.
The NME report includes DNA types for a panel of 8 markers selected from the International Society of Animal Genetics (ISAG) canine parentage panel. These markers provide individual identification for each sample tested.
While a genetic marker and test are available to identify those dogs which may be carriers, there is still ongoing research which you can help with.
Dr. Renee Barber (contact information is below) is currently conducting research at the University of Georgia. The scientific name for PDE is now necrotizing meningoencephalitis (NME) because as research has progressed, we now know that not only is the Pug breed at risk, but also the Maltese, Chihuahua, Shih Tzu, Lhasa Apso, Boston Terrier, Papillion, Pekingese, Pomeranian, Yorkshire Terrier and West Highland White Terrier breeds. This is a disease that causes inflammation in the brain which can lead to seizures, blindness, coma and death very quickly. Learning more about what causes this devastating disease is critical for helping advance diagnosis, treatment and hopefully eradication of NME. Dr. Kimberly Greer has been instrumental in finding a region of DNA that is often different in Pugs that get NME, allowing for development of a genetic test. However, there is a still a subset of Pugs that don’t have this genetic difference that will succumb to NME. Dr. Barber has devoted her current research to trying to determine why this happens.
Additionally, Dr. Barber has also identified a second region of DNA that may contribute to Pugs getting NME. She is currently working to learn more about this region. Dr. Barber is always looking for additional samples from healthy Pugs or Pugs with NME to help with their research efforts. If you have a healthy purebred Pug that is over 3 years old and would be interested in participating, your veterinarian would have to verify that your pet does not have any evidence of autoimmune or neurological disease and we will send you a kit to collect a small amount of saliva. If you are interested in participating, please contact Dr. Renee Barber at [email protected] and she will help coordinate sample collection and shipping.
Also, if you believe your Pug may be suffering from NME, please let Dr. Barber know. If your pet passes away from PDE, arrangements can be made for a veterinary pathologist to examine the brain tissue and confirm a diagnosis of NME while still allowing your pet to be cremated and returned to you. Download this file for the Protocol for PDE Necropsy Donations.
The Pug Dog Club of America recognizes how devastating the diagnosis of PDE can be and it has been our goal to support and fund research so that we can see an end to this fatal disease. We thank you for your interest in participating in this research at this most difficult time.
If you would like to make a monetary donation for ongoing research in Pug health, you can send a donation to:
Canine Health Foundation
251 West Garfield Rd. Suite, 160
Aurora, OH 44202
Please specify that your donation is for the “Pug Club Donor Advised Fund.”
Thankfully we have not had to deal with PDE at Pickwick Pugs but it is a problem unique to the Pug breed which we have been told is horrific to see and watch striking terror in the hearts of those of us who know and love them. PDE is a fatal inflammatory brain disease. We do not know exactly why Pugs get it. We are beginning to explore ways to treat it. There is no way to determine with accuracy if your Pug has it except with the brain tissue of dead dogs. The Pugs who are affected are usually young. The dogs will have seizures, circling, blindness, coma and death, all in the space of a few days to a few weeks. The Pug Dog Club of America, along with the American Kennel Club Canine Health Foundation, has contributed to studies which has directly led to the creation of a test for the genetic marker for PDE – or NME, Necrotizing Meningoencephalitis, as it is scientifically called. This is the first step towards identifying, understanding, treating and possibly eradicating this horrible disease from our Pug population.
At the 2023 Pug Dog Club of America National Conference, 3 of our pugs participated in an ongoing study being conducted (blog here) as healthy examines. They tested well and showed no early signs of PDE but they will continue to be tracked over the years. The more pugs involved in the study the more successful the data so contact contact Dr. Barber (see below) if you would like to participate and help.
Diagnosis:
According to UC Davis, www.vgl.ucdavis.edu/services/PDE.php , there is NO DIAGNOSTIC FOR PDE OR NME in dogs. There is only a test is only to determine ~RISK~ for developing NME in Pug Dogs and for selecting matings that will produce puppies that are at decreased risk (N/N, N/S). Although a significant proportion (11%) of Pug Dogs is S/S, only about 1 in 8 of this group will develop NME during their lifetime. Also, breeders are advised against breeding out the S genotype, because 40% of Pug Dogs have the S genotype in a heterozygous (N/S = 29%) or homozygous state (S/S = 11%). Eliminating the S genotype will lead to a considerable loss of genetic diversity. Therefore, breeders should carefully select matings that do not produce S/S puppies.
The NME report includes DNA types for a panel of 8 markers selected from the International Society of Animal Genetics (ISAG) canine parentage panel. These markers provide individual identification for each sample tested.
While a genetic marker and test are available to identify those dogs which may be carriers, there is still ongoing research which you can help with.
Dr. Renee Barber (contact information is below) is currently conducting research at the University of Georgia. The scientific name for PDE is now necrotizing meningoencephalitis (NME) because as research has progressed, we now know that not only is the Pug breed at risk, but also the Maltese, Chihuahua, Shih Tzu, Lhasa Apso, Boston Terrier, Papillion, Pekingese, Pomeranian, Yorkshire Terrier and West Highland White Terrier breeds. This is a disease that causes inflammation in the brain which can lead to seizures, blindness, coma and death very quickly. Learning more about what causes this devastating disease is critical for helping advance diagnosis, treatment and hopefully eradication of NME. Dr. Kimberly Greer has been instrumental in finding a region of DNA that is often different in Pugs that get NME, allowing for development of a genetic test. However, there is a still a subset of Pugs that don’t have this genetic difference that will succumb to NME. Dr. Barber has devoted her current research to trying to determine why this happens.
Additionally, Dr. Barber has also identified a second region of DNA that may contribute to Pugs getting NME. She is currently working to learn more about this region. Dr. Barber is always looking for additional samples from healthy Pugs or Pugs with NME to help with their research efforts. If you have a healthy purebred Pug that is over 3 years old and would be interested in participating, your veterinarian would have to verify that your pet does not have any evidence of autoimmune or neurological disease and we will send you a kit to collect a small amount of saliva. If you are interested in participating, please contact Dr. Renee Barber at [email protected] and she will help coordinate sample collection and shipping.
Also, if you believe your Pug may be suffering from NME, please let Dr. Barber know. If your pet passes away from PDE, arrangements can be made for a veterinary pathologist to examine the brain tissue and confirm a diagnosis of NME while still allowing your pet to be cremated and returned to you. Download this file for the Protocol for PDE Necropsy Donations.
The Pug Dog Club of America recognizes how devastating the diagnosis of PDE can be and it has been our goal to support and fund research so that we can see an end to this fatal disease. We thank you for your interest in participating in this research at this most difficult time.
If you would like to make a monetary donation for ongoing research in Pug health, you can send a donation to:
Canine Health Foundation
251 West Garfield Rd. Suite, 160
Aurora, OH 44202
Please specify that your donation is for the “Pug Club Donor Advised Fund.”
Pug Vaccinations
Visit The Pug Dog Club of America's website for recommendations on vaccinations with pugs. They cannot tolerate all vaccines and some pug owners claim that their pug died or had severe reactions (i.e. lepto). Read more here.
Visit The Pug Dog Club of America's website for recommendations on vaccinations with pugs. They cannot tolerate all vaccines and some pug owners claim that their pug died or had severe reactions (i.e. lepto). Read more here.
Porcupines and Skunks
Using tweezers or pliers, twist quills one full turn and pull out. Apply hydrogen peroxide to bleeding wounds. For skunk spray, wash dog in tomato juice. WARNING! Get your pug to a veterinarian soonest for severe bites, wounds, burns, poisoning, fits, and shocks!
Using tweezers or pliers, twist quills one full turn and pull out. Apply hydrogen peroxide to bleeding wounds. For skunk spray, wash dog in tomato juice. WARNING! Get your pug to a veterinarian soonest for severe bites, wounds, burns, poisoning, fits, and shocks!